No, amoxicillin and ampicillin are not identical, although they share similarities. They both belong to the penicillin family and fight bacterial infections by interfering with bacterial cell wall synthesis. However, subtle differences exist in their chemical structures, leading to variations in their effectiveness against specific bacteria and their absorption rates.
Amoxicillin boasts better oral absorption than ampicillin, meaning more of the drug reaches the bloodstream after ingestion. This translates to potentially higher efficacy for certain infections. Ampicillin, on the other hand, demonstrates stronger activity against some bacterial strains, such as Salmonella and Haemophilus influenzae, compared to amoxicillin. Therefore, the choice between the two depends heavily on the specific infection being treated.
Consult your physician for accurate diagnosis and prescription. Self-medicating can be dangerous; only a healthcare professional can determine which antibiotic–amoxicillin or ampicillin–is appropriate for your condition based on its severity and the specific bacteria involved. Ignoring this advice may lead to treatment failure or the development of antibiotic resistance.
Remember: This information is for educational purposes only and does not substitute professional medical advice. Always seek guidance from a qualified healthcare provider before initiating or altering any medication regimen.
- Amoxicillin and Ampicillin: The Same or Different?
- Chemical Structure and Similarities
- Impact of Side Chain Variation
- Mechanism of Action: How They Fight Infections
- Spectrum of Activity: What Bacteria They Target
- Gram-Positive Coverage Differences
- Gram-Negative Limitations
- Pharmacokinetic Differences: Absorption, Distribution, and Elimination
- Absorption
- Distribution
- Elimination
- Summary of Key Differences
- Clinical Use: Where Each Antibiotic Excels
- Side Effects and Adverse Reactions: Comparing Risks
- Gastrointestinal Issues
- Allergic Reactions
- Other Side Effects
- Choosing the Right Antibiotic: When to Use Amoxicillin vs. Ampicillin
Amoxicillin and Ampicillin: The Same or Different?
While both amoxicillin and ampicillin are penicillin antibiotics, treating similar bacterial infections, they are not identical. Key differences lie in their chemical structures and resulting properties.
Amoxicillin is a semi-synthetic penicillin, meaning it’s a modified version of naturally occurring penicillin. Ampicillin is also semi-synthetic, but with a different chemical modification. This leads to variations in how they are absorbed, distributed, and metabolized in the body.
Here’s a table summarizing key distinctions:
| Feature | Amoxicillin | Ampicillin |
|---|---|---|
| Absorption | Better absorbed orally | Lower oral bioavailability |
| Acid Stability | More stable in stomach acid | Less stable in stomach acid |
| Spectrum of Activity | Broad-spectrum, effective against Gram-positive and some Gram-negative bacteria | Broad-spectrum, similar to amoxicillin, but with some differences in bacterial coverage |
| Side Effects | Similar side effects profile to ampicillin, including diarrhea, nausea, rash | Similar side effects profile to amoxicillin, including diarrhea, nausea, rash |
The choice between amoxicillin and ampicillin depends on several factors, including the specific type of infection, patient’s medical history, and drug allergies. A doctor will determine the most appropriate antibiotic for your individual needs.
Consult your physician for accurate diagnosis and treatment. Self-medicating can be dangerous; always follow medical advice regarding antibiotic use.
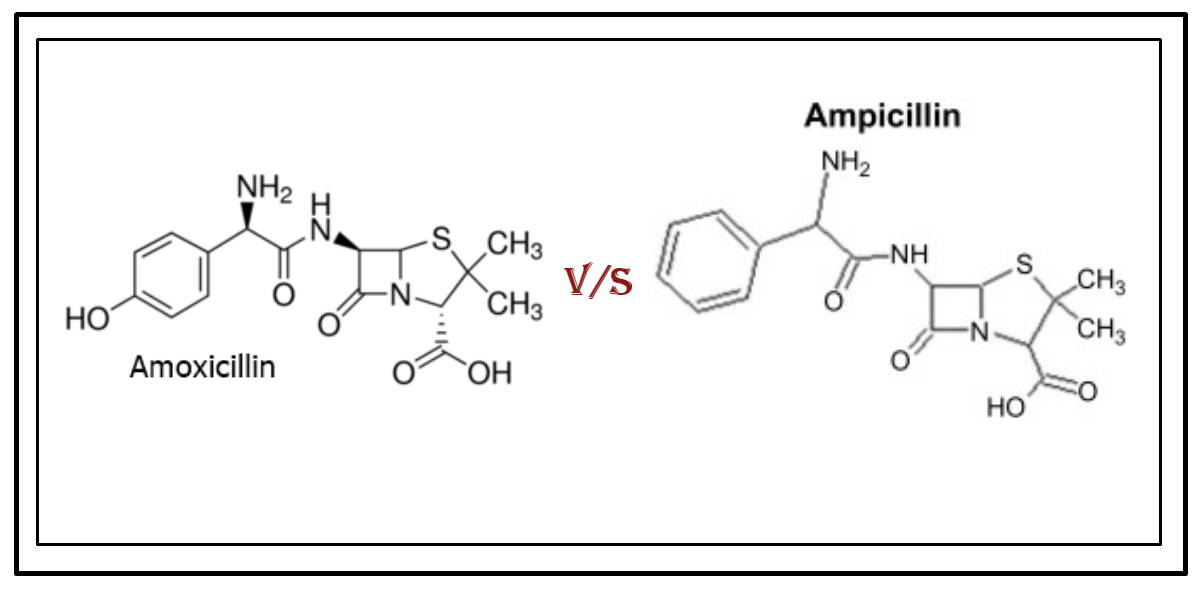
Chemical Structure and Similarities
Amoxicillin and ampicillin share a common core structure: the 6-aminopenicillanic acid (6-APA) nucleus. This nucleus forms the foundation of both antibiotics, accounting for their similar mechanisms of action. The key difference lies in the side chain attached to the 6-APA nucleus. Amoxicillin features an α-amino-p-hydroxybenzyl side chain, while ampicillin possesses an α-aminobenzyl side chain. This seemingly small alteration significantly impacts their properties.
Impact of Side Chain Variation
The differing side chains affect the antibiotics’ absorption, distribution, metabolism, and excretion (ADME) profiles. Amoxicillin demonstrates superior acid stability compared to ampicillin, leading to better oral bioavailability. Conversely, ampicillin displays broader penetration into the cerebrospinal fluid. These variations mean that although both target similar bacterial cell wall synthesis, they might be preferred for different infections.
Both antibiotics exhibit similar antimicrobial activity against Gram-positive and some Gram-negative bacteria. They inhibit bacterial cell wall synthesis by binding to penicillin-binding proteins (PBPs). However, differences in their side chains influence their affinity for specific PBPs and, consequently, their spectrum of activity against particular bacterial strains. For example, ampicillin might be more effective against certain types of Escherichia coli than amoxicillin.
Mechanism of Action: How They Fight Infections
Amoxicillin and ampicillin are both penicillin-based antibiotics. They work by inhibiting bacterial cell wall synthesis. Specifically, they target penicillin-binding proteins (PBPs), enzymes crucial for creating peptidoglycan, a major component of bacterial cell walls.
Disrupting peptidoglycan production weakens the bacterial cell wall, leading to osmotic instability. This means the bacteria cannot regulate the flow of water and essential nutrients across their membranes. The result? Cell lysis and bacterial death.
While both target PBPs, subtle differences exist in their binding affinities to various PBPs, leading to slightly varied antibacterial spectra. Amoxicillin generally demonstrates better absorption after oral administration compared to ampicillin.
Ampicillin, however, exhibits broader activity against certain bacteria, including some Gram-negative species, compared to amoxicillin. Doctors consider these differences when selecting the appropriate antibiotic for a specific infection.
Understanding this mechanism of action helps highlight the importance of appropriate antibiotic use, following prescribed dosages, and completing the full course of treatment to ensure effective eradication of bacteria and prevent the development of antibiotic resistance.
Spectrum of Activity: What Bacteria They Target
Amoxicillin and ampicillin are both aminopenicillin antibiotics, meaning they target similar bacteria. They effectively treat infections caused by Gram-positive bacteria, including Streptococcus pneumoniae (a common cause of pneumonia and ear infections), Staphylococcus aureus (responsible for skin infections and more serious illnesses), and various Streptococcus species causing strep throat and other infections. Ampicillin boasts slightly broader coverage against some Gram-negative bacteria compared to amoxicillin, such as Haemophilus influenzae (a bacteria causing respiratory tract infections) and Escherichia coli (a common cause of urinary tract infections).
Gram-Positive Coverage Differences
While both antibiotics work against many Gram-positive bacteria, subtle variations exist. Ampicillin may exhibit slightly better activity against certain strains of Enterococcus species, although resistance is increasingly prevalent. Amoxicillin might demonstrate better penetration into certain tissues, leading to more effective treatment in specific infections.
Gram-Negative Limitations
Neither amoxicillin nor ampicillin is highly effective against many Gram-negative bacteria. Their activity is often limited to certain strains, and resistance is a significant concern. Pseudomonas and other resistant strains frequently require different antibiotic choices.
Pharmacokinetic Differences: Absorption, Distribution, and Elimination
Amoxicillin and ampicillin share similarities, but key pharmacokinetic differences exist. Let’s explore absorption, distribution, and elimination.
Absorption
- Amoxicillin: Generally exhibits better oral absorption than ampicillin, reaching peak plasma concentrations faster.
- Ampicillin: Susceptible to degradation by stomach acid, leading to lower bioavailability compared to amoxicillin. Food can further reduce its absorption.
Consequently, amoxicillin often requires lower doses for comparable therapeutic effects.
Distribution
- Both: Widely distribute throughout body fluids, including cerebrospinal fluid (CSF), although penetration is limited in the presence of inflammation. They reach therapeutic levels in most tissues.
- Differences: Specific tissue distribution may vary slightly depending on factors like protein binding. Ampicillin displays higher protein binding than amoxicillin. This difference can subtly affect free drug concentrations available for action.
Elimination
- Primary Route: Renal excretion is the primary route for both drugs. About 80% of amoxicillin and a similar percentage of ampicillin are excreted unchanged in urine.
- Half-life: Amoxicillin typically has a slightly shorter half-life than ampicillin, meaning its elimination is faster.
- Dosage Adjustments: Dosage adjustments are necessary for patients with renal impairment for both medications; however, due to the differences in elimination half-life, adjustments might differ slightly.
Summary of Key Differences
Remember, these are generalizations, and individual responses to these antibiotics can vary. Always consult prescribing information for specific details.
Clinical Use: Where Each Antibiotic Excels
Amoxicillin generally boasts better oral absorption, making it the preferred choice for many common infections treatable via oral administration. This translates to higher patient compliance, as fewer pills are needed to reach therapeutic levels.
Ampicillin, however, excels in treating certain infections where its broader spectrum of activity proves advantageous. Consider these examples:
| Infection Type | Antibiotic Preference | Reason |
|---|---|---|
| Meningitis (caused by Listeria monocytogenes) | Ampicillin | Ampicillin demonstrates superior activity against this pathogen compared to amoxicillin. |
| Some Salmonella and Shigella infections | Ampicillin | Ampicillin’s broader spectrum often provides better coverage against these gram-negative bacteria. |
| Intra-abdominal infections (in specific cases) | Ampicillin (often in combination therapy) | Ampicillin, sometimes in combination with other agents, can be part of a successful treatment regimen. |
Ultimately, the choice hinges on the specific infection, patient factors, and antimicrobial susceptibility testing results. Always consult a medical professional for accurate diagnosis and treatment recommendations. This information serves for educational purposes only and should not be substituted for professional medical advice.
Side Effects and Adverse Reactions: Comparing Risks
Both amoxicillin and ampicillin belong to the penicillin family, sharing similar mechanisms but differing slightly in their side effect profiles. While both can cause gastrointestinal upset like diarrhea or nausea, ampicillin shows a higher incidence of skin rashes. Approximately 10% of patients taking ampicillin experience a rash, compared to a lower percentage with amoxicillin. This difference is significant for patients with a history of penicillin allergies.
Gastrointestinal Issues
Both antibiotics can disrupt gut flora, leading to diarrhea. Amoxicillin-related diarrhea is generally milder. However, severe cases of Clostridium difficile infection, a serious complication causing colitis, are possible with either antibiotic. Always inform your doctor if you experience persistent or bloody diarrhea.
Allergic Reactions
Serious allergic reactions, including anaphylaxis, are rare but possible with both drugs. Symptoms can range from hives and itching to difficulty breathing and swelling. Ampicillin carries a slightly higher risk of allergic reactions, particularly skin rashes. Patients with a penicillin allergy should exercise caution and discuss alternatives with their doctor before using either medication.
Other Side Effects
Less common side effects include headaches, dizziness, and changes in blood counts. These are generally mild and temporary. However, any unusual symptoms should be reported to a healthcare provider. Remember, this information isn’t a substitute for professional medical advice. Always consult your doctor or pharmacist before starting or stopping any medication.
Choosing the Right Antibiotic: When to Use Amoxicillin vs. Ampicillin
Generally, amoxicillin is preferred for most infections due to its better oral absorption and lower side effect profile.
However, ampicillin might be a better choice in specific situations:
- Severe infections: Ampicillin’s broader spectrum might be necessary for serious bacterial infections where amoxicillin’s effectiveness is questionable. This often includes infections like meningitis or endocarditis. Consult a doctor; they’ll determine the severity.
- Intravenous administration needed: Ampicillin is available in intravenous formulations, making it suitable for patients requiring rapid or continuous drug delivery, something amoxicillin doesn’t readily offer.
- Specific bacterial strains: Ampicillin shows efficacy against certain bacteria that are less susceptible to amoxicillin, particularly some strains of Listeria and Salmonella.
- Penicillin allergies (with caveats): While both are penicillins, some individuals allergic to amoxicillin can tolerate ampicillin (though cross-reactivity is possible, requiring careful medical supervision).
Amoxicillin’s advantages include:
- Better oral bioavailability: Amoxicillin is absorbed more readily after oral administration.
- Lower side effect incidence: Generally, it causes fewer gastrointestinal issues.
- Suitable for many common infections: It effectively treats many common bacterial infections like ear infections, strep throat, and urinary tract infections.
Ultimately, the choice hinges on individual patient factors and the specific infection. Always consult a healthcare professional for diagnosis and treatment. They will consider your medical history, the type of infection, and the results of any tests to prescribe the most appropriate antibiotic.