Never take amoxicillin without first consulting your doctor if you’re already on warfarin. This antibiotic can significantly alter how your body processes warfarin, increasing your risk of bleeding. Regular monitoring of your INR (International Normalized Ratio) is absolutely necessary during and after amoxicillin treatment.
Amoxicillin, a common antibiotic, interacts with warfarin, a blood thinner, by impacting gut bacteria responsible for vitamin K metabolism. Reduced vitamin K availability leads to decreased warfarin metabolism, resulting in elevated INR levels. This heightened anticoagulant effect raises your chances of experiencing spontaneous bleeding, bruising, or even more serious hemorrhagic complications.
Your doctor will likely adjust your warfarin dosage to mitigate this interaction. Expect frequent blood tests to track your INR, ensuring it remains within the therapeutic range. Closely monitor yourself for signs of bleeding, such as unusual bruising, nosebleeds, or dark stools. Report any concerns immediately to your physician. Proactive communication and vigilant monitoring are key to safe concurrent use.
Remember: This information is for general knowledge and doesn’t replace professional medical advice. Always discuss medication interactions with your doctor or pharmacist before making any changes to your treatment plan. Your health and safety are paramount.
- Amoxicillin and Warfarin: A Detailed Look at Drug Interactions
- Understanding the Risk
- Practical Recommendations
- Alternative Antibiotic Options
- Understanding Warfarin’s Mechanism of Action
- Impact on Clotting Factors
- Clinical Significance
- Amoxicillin’s Impact on Gut Flora
- The Role of Vitamin K in Blood Clotting
- The Coagulation Cascade and Vitamin K’s Role
- Vitamin K Deficiency and its Impact
- How Amoxicillin Affects Vitamin K Production
- Indirect Effects on Vitamin K Levels
- Clinical Significance Regarding Warfarin
- Recommendations
- Further Research
- Increased Risk of Bleeding: Recognizing the Symptoms
- Monitoring INR Levels During Concomitant Use
- Frequency of INR Testing
- Responding to INR Changes
- Additional Recommendations
- Important Note:
- Adjusting Warfarin Dosage: A Physician’s Role
- Alternative Antibiotics: Safer Options for Warfarin Users
- Safer Choices for Your Consideration
Amoxicillin and Warfarin: A Detailed Look at Drug Interactions
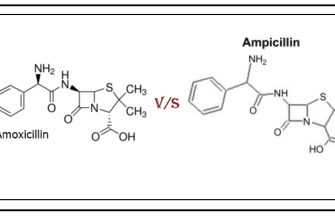
Amoxicillin, a common antibiotic, can interact with warfarin, a blood thinner, increasing your risk of bleeding. This happens because amoxicillin can alter gut bacteria, reducing vitamin K production. Vitamin K is crucial for blood clotting, and warfarin works by inhibiting vitamin K. Therefore, amoxicillin’s impact on vitamin K levels can intensify warfarin’s effects.
Understanding the Risk
The interaction’s severity varies. Some individuals experience no noticeable changes, while others see a significant increase in their INR (International Normalized Ratio), a measure of blood clotting time. Regular INR monitoring is crucial during and after amoxicillin treatment if you’re on warfarin.
Practical Recommendations
Your doctor should adjust your warfarin dosage if you need amoxicillin. This ensures your INR remains within the therapeutic range, minimizing bleeding risk. Closely monitor for signs of bleeding, such as unusual bruising, nosebleeds, or dark stools. Report any unusual bleeding to your doctor immediately. Consider keeping a medication log and documenting any changes to your routine or symptoms to aid your physician.
Alternative Antibiotic Options
If possible, your doctor may explore alternative antibiotics with less interaction potential with warfarin. This discussion should happen before initiating amoxicillin treatment. Open communication with your healthcare provider is paramount for managing this interaction successfully.
Understanding Warfarin’s Mechanism of Action
Warfarin inhibits vitamin K epoxide reductase, a crucial enzyme in the vitamin K cycle. This enzyme is responsible for recycling vitamin K, a cofactor needed for the activation of several clotting factors: II, VII, IX, and X. By blocking this enzyme, warfarin prevents the activation of these clotting factors.
Impact on Clotting Factors
The reduced activation of factors II, VII, IX, and X directly impacts the coagulation cascade. This leads to a decrease in prothrombin (Factor II) and other clotting factor levels, resulting in a prolonged clotting time. This effect is carefully monitored through regular INR (International Normalized Ratio) tests to maintain a therapeutic anticoagulant effect while minimizing bleeding risks.
Clinical Significance
This mechanism is highly relevant for patients on warfarin therapy, as it directly affects their risk of both thrombosis (blood clots) and bleeding. Careful monitoring of INR levels is paramount to ensure the balance between preventing clot formation and avoiding excessive bleeding. Dosage adjustments are frequently made based on INR results, diet, and other medications the patient may be taking.
Amoxicillin’s Impact on Gut Flora
Amoxicillin, a broad-spectrum antibiotic, disrupts the delicate balance of your gut microbiome. This disruption primarily stems from its non-specific action against a wide range of bacteria, including beneficial gut flora. This can lead to a decrease in beneficial bacteria like Bifidobacteria and Lactobacilli.
Specifically, studies show a reduction in bacterial diversity and an increase in antibiotic-resistant bacteria after amoxicillin treatment. The severity depends on factors like dosage, treatment duration, and individual gut microbial composition.
This imbalance can manifest in various ways. You might experience diarrhea, abdominal cramping, or bloating. In some cases, more severe complications such as Clostridioides difficile infection (C. diff) can occur. C. diff thrives when beneficial gut bacteria are suppressed.
To mitigate these effects, consider supplementing with probiotics during and after amoxicillin treatment. Probiotics contain live microorganisms intended to restore gut health. However, consult your doctor before taking probiotics, especially if you have a weakened immune system.
A balanced diet rich in prebiotics – substances that feed beneficial bacteria – can also help support recovery. Prebiotics are found in foods like bananas, onions, and garlic.
Regular bowel movements are crucial during and following antibiotic treatment. Maintaining hydration helps promote healthy gut function.
Remember: This information is for educational purposes only and does not constitute medical advice. Always consult your physician before starting or stopping any medication or supplement, particularly if you are also taking warfarin.
The Role of Vitamin K in Blood Clotting
Vitamin K is crucial for blood clotting. It acts as a cofactor for enzymes that modify certain clotting factors, specifically factors II, VII, IX, and X, and proteins C and S. These modified factors are then able to participate in the coagulation cascade, a complex series of reactions that ultimately lead to the formation of a stable blood clot, preventing excessive bleeding.
The Coagulation Cascade and Vitamin K’s Role
The coagulation cascade involves a precise sequence of protein activations. Vitamin K facilitates this process by enabling the carboxylation of glutamate residues within these clotting factors. This carboxylation process is what allows these proteins to bind to calcium ions, a necessary step for their proper functioning within the coagulation cascade. Without Vitamin K, these factors remain inactive, impeding clot formation.
Vitamin K Deficiency and its Impact
Insufficient Vitamin K intake or impaired absorption can significantly affect blood clotting. This can lead to increased bleeding risk, manifesting as easy bruising, prolonged bleeding from cuts, or even more severe hemorrhagic events. Individuals taking anticoagulant medications, such as warfarin, require careful monitoring of their Vitamin K intake, as warfarin’s mechanism of action involves inhibiting Vitamin K’s role in clotting factor activation. A balanced diet including leafy green vegetables, which are rich in Vitamin K, or supplements, under physician supervision, can help maintain appropriate levels.
How Amoxicillin Affects Vitamin K Production
Amoxicillin doesn’t directly affect vitamin K production in the body. Vitamin K is primarily produced by gut bacteria, and amoxicillin is a broad-spectrum antibiotic impacting various gut bacteria. This means it can disrupt the gut’s microbiome, potentially reducing vitamin K synthesis.
Indirect Effects on Vitamin K Levels
- Reduced Bacterial Synthesis: Amoxicillin’s disruption of gut flora decreases the number of bacteria producing vitamin K, potentially leading to lower vitamin K levels.
- Malabsorption: While less common, amoxicillin-induced diarrhea or gut inflammation can interfere with vitamin K absorption from food.
The extent of this reduction depends on factors like the dosage, duration of amoxicillin treatment, individual gut microbiome composition, and diet.
Clinical Significance Regarding Warfarin
The reduction in vitamin K production is important to consider if you are taking warfarin, a blood thinner whose effectiveness depends on vitamin K levels. Lower vitamin K levels increase warfarin’s effect, potentially leading to increased bleeding risk.
Recommendations
- Monitor INR: Closely monitor your International Normalized Ratio (INR) while taking amoxicillin, particularly if you’re also on warfarin. This monitors how well your blood clots.
- Dietary Considerations: Maintain a diet rich in vitamin K-containing foods like leafy green vegetables to compensate for potentially reduced production.
- Consult your doctor: Inform your physician if you’re taking both amoxicillin and warfarin. They can adjust your warfarin dosage if necessary based on your INR.
Further Research
More research is needed to fully understand the interplay between amoxicillin, gut microbiota, vitamin K production, and warfarin’s anticoagulant effect. Individual responses vary significantly.
Increased Risk of Bleeding: Recognizing the Symptoms
Amoxicillin and warfarin together increase your risk of bleeding. Know the signs!
Look for unusual bleeding, even minor. This includes:
- Frequent nosebleeds
- Easy bruising (purpura)
- Bleeding gums
- Dark or bloody urine or stools
- Heavy menstrual bleeding
- Prolonged bleeding from cuts
Internal bleeding is more serious and needs immediate medical attention. Symptoms can be subtle:
- Unexplained fatigue
- Dizziness or lightheadedness
- Weakness
- Shortness of breath
- Abdominal pain
- Headache
If you experience any of these, contact your doctor immediately. Early detection is key.
| Symptom | Description | Action |
|---|---|---|
| Unusual Bleeding | Nosebleeds, bruising, bleeding gums, etc. | Contact your doctor |
| Internal Bleeding Signs | Fatigue, dizziness, weakness, shortness of breath, abdominal pain | Seek immediate medical attention |
Remember to always inform your doctor about all medications you are taking, including over-the-counter drugs and supplements.
Monitoring INR Levels During Concomitant Use
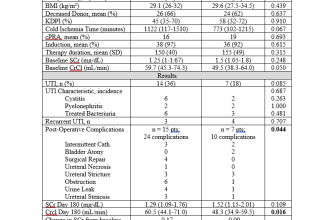
Closely monitor your INR (International Normalized Ratio) levels throughout amoxicillin and warfarin co-administration. Frequency depends on your individual risk factors, but increased monitoring is generally advised.
Frequency of INR Testing
- Increased frequency in the first week: Consider INR testing 2-3 times per week during the initial week of concurrent therapy. This allows for quick adjustments to warfarin dosage.
- Regular monitoring thereafter: After the first week, adjust testing frequency based on your physician’s recommendations and INR stability. Many patients require weekly monitoring, while others may need it less often.
- Consider individual risk factors: Factors like age, comorbidities, and previous INR instability influence monitoring frequency. Discuss your specific needs with your doctor.
Responding to INR Changes
- INR increase: If your INR increases significantly (above the therapeutic range), your doctor may reduce your warfarin dose. Report any bleeding symptoms immediately.
- INR decrease: A decrease in INR (below the therapeutic range) may require an increase in your warfarin dose. However, this is less common with amoxicillin.
- Communicate with your doctor: Always inform your physician of any changes in your INR levels or bleeding symptoms. Immediate communication helps ensure safe and effective management.
Additional Recommendations
Maintain consistent warfarin intake. Avoid significant dietary changes that could affect vitamin K levels. Report any new medications or supplements to your healthcare provider. Regular blood tests are crucial for managing this interaction.
Important Note:
This information is for educational purposes and does not replace professional medical advice. Always consult with your doctor or pharmacist before making any changes to your medication regimen.
Adjusting Warfarin Dosage: A Physician’s Role
Closely monitor INR levels. Target INR range depends on the indication for warfarin therapy. For example, patients with atrial fibrillation often aim for an INR between 2.0 and 3.0.
Reduce Warfarin dose if INR is above the therapeutic range. The amount of reduction depends on the severity of the elevation and individual patient factors. Consider temporarily suspending warfarin if INR is significantly elevated and bleeding risk is high.
Increase the Warfarin dose if INR is below the therapeutic range. Small adjustments are usually sufficient to achieve the desired INR. Patient adherence to medication and dietary intake (vitamin K-rich foods) significantly impact effectiveness.
Regularly schedule follow-up appointments for INR testing and dosage adjustments. Frequency depends on patient stability and response to therapy. Frequent monitoring is necessary initially, then gradually less frequent checks can be implemented if the INR is stable.
Consider co-morbidities and concomitant medications when adjusting Warfarin. Many drugs interact with warfarin and can alter its effects. Amoxicillin, for instance, may increase the risk of bleeding by enhancing warfarin’s anticoagulant effect. Account for these interactions in dosage adjustments.
Educate patients about the importance of consistent medication adherence, regular follow-up visits, and reporting any unusual bleeding or bruising. Patient education is paramount to successful management of warfarin therapy.
Document all dosage adjustments, INR values, and any relevant clinical findings meticulously. This ensures comprehensive patient record keeping and facilitates better future management.
Utilize clinical decision support tools and resources to optimize Warfarin dosage adjustments. These tools can assist in predicting drug interactions and guiding dosage modifications.
Always prioritize patient safety and individualized therapy. Dosage adjustments should be tailored to each patient’s unique circumstances and response to treatment.
Alternative Antibiotics: Safer Options for Warfarin Users
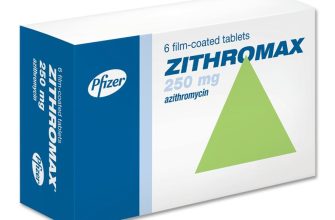
Consult your doctor immediately before changing any medication, including antibiotics. They can assess your specific situation and recommend the safest course of action. While amoxicillin can interact negatively with warfarin, increasing bleeding risk, several alternatives generally pose a lower risk.
Safer Choices for Your Consideration
Clinicians often prescribe antibiotics from the following classes when managing patients on warfarin: Cefazolin, a first-generation cephalosporin, and clindamycin, a lincosamide, are frequently selected because they demonstrate a lower propensity for interactions with warfarin than amoxicillin. Your physician will consider your infection type, sensitivity tests, and your overall health when choosing the most suitable antibiotic. Azithromycin, a macrolide, may also be considered; however, it’s crucial to closely monitor your INR levels (International Normalized Ratio) while taking it, as some individuals may experience increased INR.
Remember, careful INR monitoring is vital regardless of the antibiotic chosen. Regular blood tests will allow your doctor to adjust your warfarin dose, ensuring your blood remains within the therapeutic range and minimizes the risk of bleeding or clotting complications. Open communication with your healthcare provider is key to managing both your infection and your anticoagulation therapy safely and effectively.