Ciprofloxacin (Cipro) rarely causes significant bleeding as a direct side effect. However, it can interact with medications that do increase bleeding risk, such as blood thinners like warfarin or aspirin. This interaction is crucial to consider.
If you’re taking Cipro and experience unusual bleeding–heavy menstrual bleeding, nosebleeds, easy bruising, or bleeding from gums–contact your doctor immediately. This isn’t necessarily proof Cipro is the cause, but warrants prompt medical attention. Your doctor will assess your overall health, medication list, and bleeding symptoms to determine the next steps.
Reports of gastrointestinal bleeding are more common than other types of bleeding linked to Cipro. This is typically mild, but severe cases necessitate immediate medical care. Pre-existing digestive issues can heighten this risk. Always inform your doctor about all health conditions and medications you’re taking before starting Cipro or any new drug.
Remember, this information is for general knowledge and doesn’t replace professional medical advice. A healthcare provider can assess your specific situation and provide personalized guidance on managing potential risks associated with Ciprofloxacin use.
- Can Cipro Cause Bleeding?
- Interactions with Blood Thinners
- Other Factors Affecting Bleeding Risk
- Signs of Bleeding and When to Seek Medical Attention
- Disclaimer:
- Cipro’s Mechanism of Action and Bleeding Risk
- Reported Cases of Cipro-Related Bleeding: A Review
- Types of Bleeding Associated with Ciprofloxacin Use
- Risk Factors Increasing Cipro-Induced Bleeding
- Pre-existing Conditions
- Age and Liver/Kidney Function
- Drug Interactions
- Alcohol Consumption
- Individual Sensitivity
- How to Recognize and Respond to Cipro-Related Bleeding
- Interaction with Other Medications That May Increase Bleeding Risk
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Blood Thinners (Anticoagulants)
- Antiplatelet Drugs
- When to Consult a Doctor Regarding Cipro and Bleeding
- Specific Situations Requiring Immediate Medical Attention
- When to Schedule a Follow-up Appointment
Can Cipro Cause Bleeding?
Ciprofloxacin (Cipro) rarely causes significant bleeding as a direct side effect. However, it can indirectly increase the risk of bleeding in some situations. This is primarily due to its potential interaction with blood thinners.
Interactions with Blood Thinners
Cipro can interact with anticoagulants like warfarin (Coumadin) and some newer oral anticoagulants. This interaction can enhance the effects of these medications, increasing the risk of bleeding, bruising, or unusual bleeding episodes. If you take blood thinners, discuss Cipro use with your doctor before starting treatment. Regular blood tests might be needed to monitor your INR (International Normalized Ratio) if you’re on warfarin.
Other Factors Affecting Bleeding Risk
Other conditions or medications can also affect bleeding risk. For example, individuals with existing bleeding disorders or liver disease are more susceptible to bleeding complications. Concurrent use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, also raises the possibility of increased bleeding. Consult your doctor about all medications you are taking before starting Cipro.
Signs of Bleeding and When to Seek Medical Attention
Seek immediate medical attention if you experience unusual or heavy bleeding while taking Cipro, including nosebleeds, black stools, blood in your urine, or excessive bruising. These symptoms require prompt evaluation to determine the cause and appropriate management.
Disclaimer:
This information is for educational purposes only and should not be considered medical advice. Always consult your physician or other qualified healthcare professional for any questions you may have regarding a medical condition or treatment.
Cipro’s Mechanism of Action and Bleeding Risk
Ciprofloxacin, or Cipro, targets bacterial DNA gyrase and topoisomerase IV, enzymes crucial for bacterial DNA replication and repair. This disruption prevents bacterial growth and ultimately leads to bacterial death. The mechanism doesn’t directly involve blood clotting pathways.
However, Cipro, like many antibiotics, can disrupt gut flora. This imbalance can, in rare cases, increase the risk of vitamin K deficiency, impacting blood clotting. A vitamin K deficiency can lead to increased bleeding risk. This is not a direct effect of Cipro on blood vessels or clotting factors but an indirect consequence of its impact on gut bacteria.
While rare, reports of increased bleeding or bruising with Cipro use exist. These cases frequently involve patients with pre-existing conditions affecting blood clotting or those taking medications that influence coagulation.
Consult your doctor if you have concerns about bleeding while taking Cipro, especially if you have a bleeding disorder or take blood thinners. They can assess your individual risk and provide tailored advice.
Remember to always inform your healthcare provider about all medications and supplements you are taking to minimize potential drug interactions.
Reported Cases of Cipro-Related Bleeding: A Review
While Ciprofloxacin (Cipro) is generally considered safe, reports of bleeding complications exist. These are not common, but understanding them is vital for patient safety. Reported incidents often involve gastrointestinal bleeding, such as hematemesis (vomiting blood) or melena (dark, tarry stools).
Other less frequent bleeding occurrences include epistaxis (nosebleeds) and hematuria (blood in urine). It’s crucial to note that these incidents aren’t automatically attributed to Cipro; underlying conditions and interactions with other medications often play a significant role.
The severity of bleeding varies considerably. Some cases are mild and resolve spontaneously, while others may necessitate immediate medical attention. Factors influencing bleeding severity include the patient’s overall health, existing medical conditions (such as blood clotting disorders), and the dosage of Cipro.
| Type of Bleeding | Frequency (Approximate) | Possible Contributing Factors |
|---|---|---|
| Gastrointestinal Bleeding | Most common | Pre-existing ulcers, NSAID use, impaired clotting |
| Epistaxis | Less common | Underlying vascular conditions, trauma |
| Hematuria | Rare | Kidney issues, urinary tract infections |
If you experience any unusual bleeding while taking Cipro, contact your doctor immediately. Thorough investigation is needed to determine causality. This might involve blood tests to assess clotting factors, endoscopic procedures to examine the gastrointestinal tract, or other diagnostic tests depending on the nature of the bleeding.
This information provides a general overview. Always consult your healthcare provider for personalized advice and management of any bleeding concerns.
Types of Bleeding Associated with Ciprofloxacin Use
While Ciprofloxacin (Cipro) rarely causes bleeding, it’s crucial to understand the potential types. Reports suggest a link to several bleeding complications, though more research is needed to fully establish causal relationships.
- Gastrointestinal Bleeding: This manifests as blood in vomit or stool, potentially ranging from mild to severe. Factors like existing ulcers or concurrent medication use may increase the risk.
- Easy Bruising (Purpura): Cipro may, in some cases, impair platelet function, leading to increased bruising with minimal trauma. Observe any unusual or excessive bruising.
- Bleeding from Cuts or Wounds: If you experience prolonged bleeding from minor injuries while taking Cipro, consult your doctor. This could indicate a clotting disorder or interaction with the medication.
It’s important to note:
- These occurrences are uncommon.
- The exact mechanisms linking Cipro to bleeding aren’t fully understood.
- Individual reactions vary considerably.
Consult your physician immediately if you experience any unusual bleeding while taking Ciprofloxacin. They can assess your situation, consider other potential causes, and adjust your treatment plan as needed. Providing a complete medical history, including other medications and pre-existing conditions, will aid in accurate diagnosis and management. Don’t self-treat or delay seeking professional medical attention.
Risk Factors Increasing Cipro-Induced Bleeding
Concurrent use of blood thinners, like warfarin or aspirin, significantly raises your risk of bleeding while taking Cipro. Close monitoring by your doctor is crucial in such cases. Regular blood tests help manage dosage and minimize this risk.
Pre-existing Conditions
Individuals with bleeding disorders, such as hemophilia or von Willebrand disease, are more susceptible to Cipro-induced bleeding. Open communication with your physician about your medical history is paramount. They can help you assess your risk and discuss alternative treatments.
Age and Liver/Kidney Function
Older adults often have reduced liver and kidney function, potentially affecting Cipro metabolism and increasing bleeding risk. Similarly, pre-existing liver or kidney disease presents a higher risk. Your doctor will carefully consider these factors before prescribing Cipro.
Drug Interactions
Beyond blood thinners, certain medications interact with Cipro, increasing bleeding potential. Always provide your doctor with a complete list of your current medications, both prescription and over-the-counter. This allows for a thorough assessment of potential interactions.
Alcohol Consumption
Excessive alcohol consumption can exacerbate the effects of Cipro, increasing the chance of bleeding complications. Moderate your alcohol intake or abstain entirely while taking Cipro. Discuss your alcohol consumption habits with your doctor.
Individual Sensitivity
Finally, remember that individual responses to medications vary. Some individuals might be more prone to Cipro-induced bleeding than others, even without identifiable risk factors. Immediate medical attention is necessary should you experience unusual bleeding. Report any concerns to your healthcare provider immediately.
How to Recognize and Respond to Cipro-Related Bleeding
Cipro-related bleeding is rare, but recognizing the signs is crucial. Look for unusual bleeding, such as:
- Nosebleeds that are frequent or unusually heavy.
- Easy bruising or the appearance of unexplained purple or red spots on your skin.
- Bleeding gums that persist after brushing or flossing.
- Blood in your urine or stool.
- Heavy or prolonged menstrual bleeding.
If you experience any of these, contact your doctor immediately. Don’t delay. Early intervention is key.
Your doctor will likely ask about your medication history and conduct a physical examination. They may also order blood tests to check your platelet count and other blood clotting factors. This helps them determine if the bleeding is indeed related to Ciprofloxacin.
Depending on the severity and cause of the bleeding, your doctor may recommend:
- Stopping Ciprofloxacin. This is a common first step.
- Medication to help your blood clot more easily.
- Monitoring your condition closely.
- In severe cases, hospitalization for blood transfusions or other treatments may be necessary.
Keep a detailed record of your symptoms and when they started. Share this information with your doctor. This helps them diagnose and treat the problem accurately. Remember, prompt action can make a significant difference.
Interaction with Other Medications That May Increase Bleeding Risk
Ciprofloxacin, while generally safe, can interact with certain medications, increasing your risk of bleeding. Always inform your doctor about all medications you are taking, including over-the-counter drugs and supplements. This proactive approach helps prevent potential complications.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs like ibuprofen and naproxen thin your blood, increasing the chance of bleeding when combined with Cipro. This heightened risk applies to both internal and external bleeding. Consult your doctor before taking NSAIDs concurrently with Cipro.
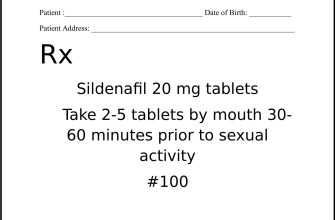
Blood Thinners (Anticoagulants)
Combining Cipro with blood thinners such as warfarin (Coumadin) or heparin significantly raises the bleeding risk. Close monitoring by your physician is vital if you must take both. Regular blood tests might be necessary to adjust your anticoagulant dosage accordingly.
Antiplatelet Drugs
Aspirin and other antiplatelet medications prevent blood clots. When taken with Cipro, this effect is amplified, leading to a higher likelihood of bleeding. Discuss alternative pain management strategies with your doctor if you’re on antiplatelet therapy.
This information is for educational purposes and does not replace professional medical advice. Always consult your healthcare provider before making any changes to your medication regimen.
When to Consult a Doctor Regarding Cipro and Bleeding
Contact your doctor immediately if you experience any bleeding while taking Cipro, especially if it’s heavy, unusual, or prolonged. This includes bleeding from your gums, nose, or any other body part. Don’t wait for the bleeding to stop on its own.
Specific Situations Requiring Immediate Medical Attention
Seek immediate medical help if you experience:
- Heavy vaginal bleeding.
- Bleeding that soaks through more than one pad or tampon per hour.
- Blood in your urine or stool.
- Unexplained bruising or pinpoint red spots on your skin.
- Bleeding accompanied by dizziness or lightheadedness.
Report any new or worsening bleeding to your healthcare provider, even if it seems minor. Your doctor can assess the situation and determine if it’s related to Cipro or another cause. Early intervention can prevent complications.
When to Schedule a Follow-up Appointment
Mild bleeding, such as slight nosebleeds or some spotting, warrants a follow-up appointment with your physician. Describe the bleeding in detail, including duration, amount, and location. Your doctor might adjust your medication or recommend other actions.