If you’re experiencing boils while taking Ciprofloxacin (Cipro), seek immediate medical attention. Don’t delay; prompt diagnosis and treatment are key to preventing complications.
Cipro, a fluoroquinolone antibiotic, can suppress the immune system, potentially increasing susceptibility to skin infections like boils. This effect varies between individuals, depending on factors such as dosage, duration of treatment, and overall health. Proper hygiene practices, such as frequent handwashing and keeping affected areas clean and dry, are crucial during Cipro use.
Boils, or furuncles, are painful, pus-filled skin infections. While many resolve on their own, those appearing during Cipro treatment may require specific medical management. Your doctor can determine the best course of action, which may include incision and drainage, antibiotic adjustments, or other supportive therapies. Carefully follow their instructions and report any worsening symptoms. Close monitoring is recommended to ensure prompt resolution and prevent further infection spread.
Remember, this information should not replace professional medical advice. Always consult your physician or other qualified healthcare provider for diagnosis and treatment of any medical condition.
- Cipro and Boils: Understanding the Connection
- When Cipro Might Be Involved
- Seeking Professional Medical Advice
- What are Boils and How Do They Develop?
- The Infection Process
- Factors Increasing Boil Risk
- Ciprofloxacin: Mechanism of Action and Uses
- Can Cipro Treat Boils? Exploring its Effectiveness
- When Cipro Might Not Be the Right Choice for Boils
- Potential Side Effects of Ciprofloxacin
- Alternative Treatments for Boils
- Prevention Strategies for Boils
- When to Seek Medical Attention for Boils
Cipro and Boils: Understanding the Connection
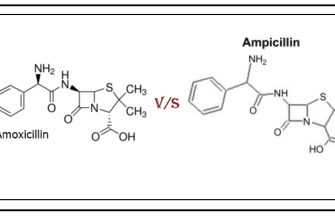
Ciprofloxacin (Cipro) is an antibiotic, not a treatment for boils. Boils are skin infections caused by bacteria, usually Staphylococcus aureus. While Cipro *can* treat some bacterial infections, it’s not always effective against the bacteria causing boils. Your doctor needs to identify the specific bacteria causing your boil to determine the appropriate treatment. Misusing antibiotics can lead to antibiotic resistance, making future infections harder to treat.
When Cipro Might Be Involved
Cipro may be prescribed if a boil becomes significantly infected or spreads, potentially requiring a broader-spectrum antibiotic. However, this is a decision made by a physician based on a thorough assessment of the infection. Drainage and proper wound care are often the primary treatments for boils. Oral antibiotics, including Cipro, are usually reserved for severe cases.
Seeking Professional Medical Advice
Never self-treat a boil. See a doctor for diagnosis and treatment. They will assess the severity of your boil, take a sample if needed to identify the bacteria, and prescribe the most suitable course of action. This may involve incision and drainage, topical antibiotics, or oral antibiotics–but not necessarily Cipro. Proper treatment minimizes complications and promotes faster healing.
What are Boils and How Do They Develop?
Boils, or furuncles, are painful, pus-filled skin infections. They arise from hair follicles or sweat glands becoming infected, usually by Staphylococcus aureus bacteria. This bacteria commonly lives on the skin without causing problems, but a break in the skin–a minor cut, abrasion, or ingrown hair–can provide an entry point.
The Infection Process
Once inside, the bacteria multiply, triggering inflammation. Your body’s immune system responds by sending white blood cells to fight the infection. This immune response causes the infected area to swell, redden, and become tender. The accumulated pus forms a central core within the boil, creating the characteristic raised bump.
Factors Increasing Boil Risk
Several factors increase your risk of developing boils. Poor hygiene can contribute to bacterial overgrowth. Weakened immune systems, such as those resulting from diabetes or HIV, make you more vulnerable. Close contact with others, particularly in crowded environments, also heightens the chance of bacterial transmission. Friction and irritation from tight clothing can also create entry points for infection.
Ciprofloxacin: Mechanism of Action and Uses
Ciprofloxacin targets bacterial DNA replication. It works by inhibiting two enzymes, topoisomerase IV and DNA gyrase, crucial for bacterial cell division and DNA repair. This inhibition prevents bacterial DNA replication and transcription, ultimately leading to bacterial cell death.
Ciprofloxacin’s broad-spectrum activity makes it effective against a wide range of bacterial infections. Common uses include:
- Respiratory tract infections (pneumonia, bronchitis)
- Skin and soft tissue infections (cellulitis, abscesses)
- Urinary tract infections (cystitis, pyelonephritis)
- Bone and joint infections (osteomyelitis)
- Gastrointestinal infections (typhoid fever)
However, its use is becoming more complicated due to increasing antibiotic resistance. Always follow a doctor’s prescription precisely, including dosage and duration.
Specific circumstances, such as allergies or other medical conditions, significantly influence Ciprofloxacin’s suitability. Consult your physician before starting any treatment.
Important side effects to be aware of include:
- Nausea
- Diarrhea
- Headache
- Muscle and tendon problems (tendinitis, tendon rupture)
Rare but serious side effects warrant immediate medical attention. These can include allergic reactions, such as hives or difficulty breathing.
Always inform your doctor about all medications you are taking to avoid potential interactions. Proper diagnosis and treatment are paramount for positive outcomes.
Can Cipro Treat Boils? Exploring its Effectiveness
Ciprofloxacin (Cipro) is not typically used to treat boils. Boils, or furuncles, are skin infections caused by bacteria, usually Staphylococcus aureus. While Cipro is an antibiotic, it’s not always the best choice for staph infections. Many strains of S. aureus have developed resistance to Cipro.
Doctors usually recommend draining a boil to promote healing. This may involve a minor surgical procedure. Antibiotics are generally reserved for more severe cases, such as large boils, recurring boils, or boils accompanied by other symptoms like fever or widespread infection. If antibiotics are deemed necessary, a doctor will select an appropriate antibiotic based on the specific bacteria causing the infection and the patient’s medical history. This often involves a culture to identify the bacteria and its susceptibility to different antibiotics.
Consider these points:
- Self-treating boils with Cipro is risky. Incorrect antibiotic use contributes to antibiotic resistance.
- Consult a doctor for proper diagnosis and treatment of a boil.
- Follow your doctor’s advice regarding treatment. This might include incision and drainage, antibiotic prescriptions tailored to the specific infection, or other measures.
Remember, seeking professional medical advice is crucial for managing a boil. Proper diagnosis ensures the most appropriate treatment plan for your specific situation.
When Cipro Might Not Be the Right Choice for Boils
Ciprofloxacin (Cipro) isn’t always the best option for boils. Consider alternatives if you have a penicillin allergy, as cross-reactivity can occur.
Avoid Cipro if you’ve experienced previous adverse reactions to fluoroquinolones. These antibiotics can cause serious side effects, including tendon rupture and peripheral neuropathy. Your doctor will weigh these risks against the benefit of treatment.
If your boil is small and uncomplicated, warm compresses and good hygiene might suffice. Simple boils often heal without antibiotics.
Severe or recurrent boils necessitate a different approach. Your doctor might prefer draining the boil surgically and prescribing a different antibiotic, like clindamycin or a cephalosporin, tailored to the specific bacteria involved.
Pregnancy and breastfeeding influence antibiotic choices. Cipro isn’t usually recommended during these periods due to potential risks to the fetus or infant. Your doctor will choose a safer antibiotic.
Underlying conditions like diabetes can affect boil treatment. Managing your blood sugar is crucial for faster healing, and your doctor might recommend more aggressive treatment than just antibiotics. Always discuss your complete medical history with your doctor before starting any medication.
Potential Side Effects of Ciprofloxacin
Ciprofloxacin, while effective, can cause various side effects. Common ones include nausea, diarrhea, and abdominal pain. These usually are mild and resolve on their own. However, report persistent or severe symptoms to your doctor immediately.
More serious, though less frequent, side effects include tendon rupture, particularly in older adults or those taking corticosteroids. This necessitates immediate medical attention if pain or swelling in a tendon occurs.
Ciprofloxacin can also impact your nervous system. You might experience dizziness, headache, or confusion. In rare instances, serious neurological reactions can develop, necessitating prompt medical intervention.
Skin reactions like rash or itching are possible. A severe allergic reaction, a medical emergency, is characterized by difficulty breathing, swelling of the face or throat, and hives. Seek immediate medical help if this happens.
Phototoxicity, increased sensitivity to sunlight, is another potential side effect. Protect yourself from prolonged sun exposure while taking Ciprofloxacin. Use sunscreen and protective clothing.
This information is not exhaustive. Consult your physician or pharmacist for a complete list of potential side effects and to discuss any concerns you may have about your treatment.
Alternative Treatments for Boils
Warm compresses are your first line of defense. Apply a warm, wet cloth to the boil for 10-15 minutes, several times a day. This increases blood flow, promoting drainage and healing.
Epsom salt soaks offer additional benefits. Dissolve Epsom salts in warm water and soak the affected area for 15-20 minutes. This helps draw out pus and reduce inflammation.
- Tea tree oil: Apply a diluted solution (mix with a carrier oil like coconut oil) directly to the boil. Its antiseptic properties can help fight infection. Always perform a patch test before widespread application.
- Aloe vera: The gel from an aloe vera plant can soothe the skin and reduce inflammation. Apply directly to the boil.
- Honey: Raw honey possesses antibacterial properties. Apply a thin layer to the boil and cover with a bandage.
Over-the-counter pain relievers, like ibuprofen or acetaminophen, can help manage pain and reduce fever.
- Maintain good hygiene. Wash the affected area gently with soap and water.
- Avoid squeezing or picking the boil. This can spread the infection.
- Keep the boil clean and covered with a sterile bandage.
Remember, these are complementary therapies. If the boil is large, extremely painful, shows signs of worsening, or doesn’t improve after a week, seek medical attention immediately. A doctor can determine the best course of action and potentially prescribe antibiotics if necessary.
Prevention Strategies for Boils
Maintain meticulous hygiene. Wash your hands frequently with soap and water, especially after touching potentially contaminated surfaces or before handling food.
Keep your skin clean and dry. Regular showering or bathing helps remove dirt and sweat, reducing bacteria buildup. Pay close attention to areas prone to friction or sweating.
Treat minor skin injuries immediately. Clean and disinfect any cuts, scrapes, or insect bites to prevent infection. Apply antibiotic ointment if needed.
Avoid sharing personal items. This includes towels, razors, and clothing. Sharing increases the risk of spreading bacteria.
Boost your immune system. A healthy immune system is better equipped to fight off infections. Eat a balanced diet, get enough sleep, and manage stress.
Control diabetes. Poorly managed diabetes increases the risk of developing boils. Work closely with your doctor to maintain healthy blood sugar levels.
Practice safe shaving techniques. Use a sharp razor and shave in the direction of hair growth to minimize skin irritation.
Wear clean clothing. Choose loose-fitting, breathable fabrics to allow proper air circulation and prevent sweat buildup.
When to Seek Medical Attention for Boils
See a doctor if your boil is larger than 1 inch in diameter, shows signs of spreading, or doesn’t improve after a week of home care. Pain that radiates, or is accompanied by fever (over 100.4°F or 38°C), chills, or swollen lymph nodes requires immediate medical attention.
Consider professional help if the boil is on your face, spine, or near your genitals. These areas are particularly sensitive, and infection can spread rapidly. Deep boils, those that appear red and swollen under the skin and don’t have a visible head, also need medical evaluation.
Repeated boils, or boils that keep returning in the same spot, might indicate an underlying medical condition, such as diabetes or a weakened immune system. A doctor can help diagnose and manage such conditions.
| Symptom | Action |
|---|---|
| Boil larger than 1 inch | See a doctor |
| Spreading infection | Seek immediate medical attention |
| No improvement after 1 week | Consult a doctor |
| Fever (over 100.4°F) | Go to the doctor immediately |
| Boil on face, spine, or near genitals | See a doctor |
| Deep boil (no visible head) | Seek medical evaluation |
| Recurring boils | Consult a doctor for underlying condition check |
Don’t hesitate to contact your healthcare provider if you have any concerns about your boil. Early intervention can prevent serious complications.