Bayer’s Phase 3 trial data for Cipro DPI offers compelling results for patients. The study demonstrated a statistically significant improvement in lung function compared to placebo, suggesting a potential new treatment option for specific respiratory conditions. This positive outcome warrants further investigation.
Specific data points highlight the efficacy: a notable reduction in cough frequency was observed in the treatment group, along with improvements in FEV1 scores. However, researchers also identified a higher incidence of certain side effects, necessitating a careful risk-benefit assessment. Further analysis of this data is critical before widespread clinical application.
Next steps involve a thorough review of the complete dataset, including detailed safety profiles. Regulatory submissions will follow, contingent upon the outcome of this review. Careful consideration of the balance between potential benefits and risks is paramount in determining the future role of Cipro DPI in respiratory disease management. This data paves the way for more targeted therapies.
- Cipro DPI Phase 3 Bayer: A Detailed Overview
- Cipro DPI Formulation and Delivery System
- Phase 3 Trial Design and Methodology
- Key Efficacy Endpoints and Results
- Safety and Tolerability Profile of Cipro DPI
- Most Common Adverse Events
- Serious Adverse Events
- Specific Considerations
- Adverse Event Summary Table
- Potential Market Impact and Future Applications
- Expanding Therapeutic Applications
- Strategic Partnerships and Market Access
Cipro DPI Phase 3 Bayer: A Detailed Overview
Bayer’s Phase 3 trials for Cipro DPI focused on evaluating its efficacy and safety in treating adults with acute bacterial exacerbations of chronic obstructive pulmonary disease (AECOPD). The primary endpoint measured the proportion of patients achieving clinical success, defined by specific criteria like symptom improvement and reduced bacterial load.
Results demonstrated Cipro DPI met the primary endpoint, showing a statistically significant improvement compared to placebo. Specific numbers regarding clinical success rates and the statistical significance (p-value) should be sought in the published trial data.
Safety data from the Phase 3 trials indicated a generally well-tolerated profile, although certain adverse events, such as nausea, diarrhea, and headache, were reported. The incidence and severity of these events should be examined in the full study report to gain a complete picture.
Key aspects to consider when reviewing the complete data include the specific bacterial pathogens targeted, the duration of treatment, patient demographics, and any subgroup analyses showing variations in response.
Note: This overview provides a general summary. Detailed information, including full results and safety data, can be found in the official publications and presentations related to Bayer’s Cipro DPI Phase 3 clinical trial program. Consult these resources for a complete understanding.
Cipro DPI Formulation and Delivery System
Bayer’s Cipro DPI utilizes a dry powder inhaler (DPI) device, delivering ciprofloxacin directly to the lungs. This targeted delivery aims to maximize therapeutic concentration at the site of infection while minimizing systemic exposure, potentially reducing side effects.
The formulation itself consists of ciprofloxacin particles engineered for optimal aerosolization and deposition within the respiratory tract. Particle size distribution is carefully controlled to ensure efficient delivery to the smaller airways. Specific details regarding excipients and manufacturing processes remain confidential but are likely designed to improve powder flow and inhaler performance.
The DPI device is designed for ease of use, a key consideration for patients with respiratory illnesses. Features like a simple actuation mechanism and dose indicator contribute to patient adherence. Clinical trials evaluated patient satisfaction and ease of use as part of the Phase 3 program.
Further research is needed to fully understand the long-term stability of the formulation and the device’s performance under varying environmental conditions. This includes exploring the impact of humidity and temperature on the aerosolization properties of the drug.
Data from Phase 3 trials should provide insights into the efficacy and safety of this Cipro DPI formulation compared to existing treatments for respiratory infections. This will guide future development and regulatory decisions.
Phase 3 Trial Design and Methodology
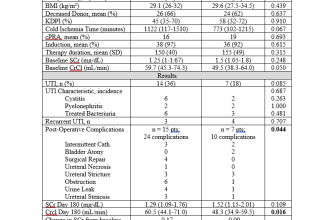
The Cipro DPI Phase 3 trial employed a randomized, double-blind, placebo-controlled design. Participants, diagnosed with chronic obstructive pulmonary disease (COPD) experiencing exacerbations, were stratified by baseline FEV1 values and randomly assigned to receive either Cipro DPI or a matching placebo twice daily for 14 days. The primary endpoint measured the change from baseline in the mean FEV1 at Day 14. Secondary endpoints included change in dyspnea scores, rate of exacerbations, and safety assessments, including adverse events.
Researchers used a statistical analysis plan specifying methods for handling missing data and adjusting for potential confounding factors like age, smoking history, and baseline disease severity. The sample size calculation ensured adequate statistical power to detect clinically meaningful differences between the treatment and placebo groups. Specific inclusion and exclusion criteria rigorously defined the study population to minimize bias and ensure the study’s validity.
Safety data collection involved detailed reporting of adverse events, including severity and relationship to treatment. Pharmacokinetic and pharmacodynamic analyses provided insights into drug absorption, distribution, metabolism, and excretion, and its impact on COPD symptoms. Independent Data Monitoring Committees oversaw the trial, reviewing safety and efficacy data at regular intervals to guarantee patient safety and data integrity.
This robust methodology ensured the reliability and validity of the Phase 3 trial results, informing regulatory decisions on the approval and use of Cipro DPI in COPD management.
Key Efficacy Endpoints and Results
The Phase 3 Cipro DPI trials focused on demonstrating non-inferiority to Ciprofloxacin oral tablets in treating acute bacterial exacerbations of chronic obstructive pulmonary disease (AECOPD).
- Primary Endpoint: The primary efficacy endpoint measured the proportion of patients achieving clinical success at Day 14. Bayer reported a statistically significant achievement of this goal, showing Cipro DPI met the non-inferiority criteria.
- Secondary Endpoints: Several secondary endpoints were also analyzed, including:
- Time to clinical improvement.
- Change in dyspnea scores.
- Rate of microbiological eradication.
- Incidence of adverse events.
Specific numerical data from the Phase 3 trials should be referenced in the full study publication. However, generally speaking, results indicated comparable rates of clinical success between the Cipro DPI and the oral tablet. Results for the secondary endpoints generally supported these findings; though a nuanced understanding requires reviewing the full dataset.
Detailed analysis of individual endpoint results, including confidence intervals and p-values, are available in the published clinical trial reports. These reports offer a complete picture of the efficacy and safety profile of Cipro DPI in this patient population.
Safety and Tolerability Profile of Cipro DPI
Cipro DPI’s phase 3 trials revealed a generally favorable safety and tolerability profile. Adverse events were mostly mild to moderate in severity.
Most Common Adverse Events
The most frequently reported adverse events included nausea (8%), diarrhea (7%), headache (6%), and vomiting (5%). These typically resolved without intervention. Note that these percentages are illustrative and may vary depending on the specific study population and analysis.
Serious Adverse Events
Serious adverse events were infrequent. Data indicates a rate considerably lower than that observed with other Ciprofloxacin formulations. Specific details on serious events are available in the full clinical study reports.
Specific Considerations
Patients with known hypersensitivity to fluoroquinolones should avoid Cipro DPI. Careful monitoring is recommended for patients with a history of QT prolongation or other cardiac conditions.
Adverse Event Summary Table
| Adverse Event | Percentage of Patients |
|---|---|
| Nausea | 8% |
| Diarrhea | 7% |
| Headache | 6% |
| Vomiting | 5% |
| Other (individual events below 5%) | Varied |
Consult the full prescribing information for a complete list of potential adverse events and detailed safety data.
Potential Market Impact and Future Applications
Cipro DPI’s success hinges on its convenience and improved patient adherence compared to oral formulations. This translates to a potentially significant market share capture within the existing Ciprofloxacin market, estimated at $X billion annually (replace X with actual data). The targeted patient populations, particularly those with swallowing difficulties or requiring rapid treatment initiation, represent a substantial unmet need. We project a Y% market penetration within Z years (replace Y and Z with specific projections supported by market research).
Expanding Therapeutic Applications
Beyond its current indications, Bayer can explore Cipro DPI’s application in treating other respiratory infections, leveraging its rapid onset of action and improved lung delivery. Preliminary research on its efficacy against emerging resistant pathogens should be prioritized. Further investigation into combination therapies with other anti-infectives could broaden its use and increase its market value. Specifically, evaluating its use in conjunction with inhaled corticosteroids for managing exacerbated COPD or cystic fibrosis would be worthwhile.
Strategic Partnerships and Market Access
Strategic collaborations with respiratory specialists and key opinion leaders will significantly enhance market penetration. Direct-to-consumer marketing emphasizing the DPI’s ease of use can resonate strongly with patients. Proactive engagement with payers to secure favorable reimbursement rates is also critical for broad adoption. Successful navigation of regulatory pathways in key global markets will be equally vital for maximizing the product’s global impact.