No, doxycycline isn’t a first-line treatment for E. coli urinary tract infections (UTIs). Doctors typically prescribe antibiotics like nitrofurantoin or trimethoprim-sulfamethoxazole initially. However, doxycycline can be a viable option in specific circumstances.
Doxycycline’s effectiveness against E. coli varies depending on antibiotic resistance patterns in your area. Your physician will consider your individual medical history, including allergies and previous antibiotic use, when selecting the right treatment. Always consult your doctor before taking any medication, including antibiotics.
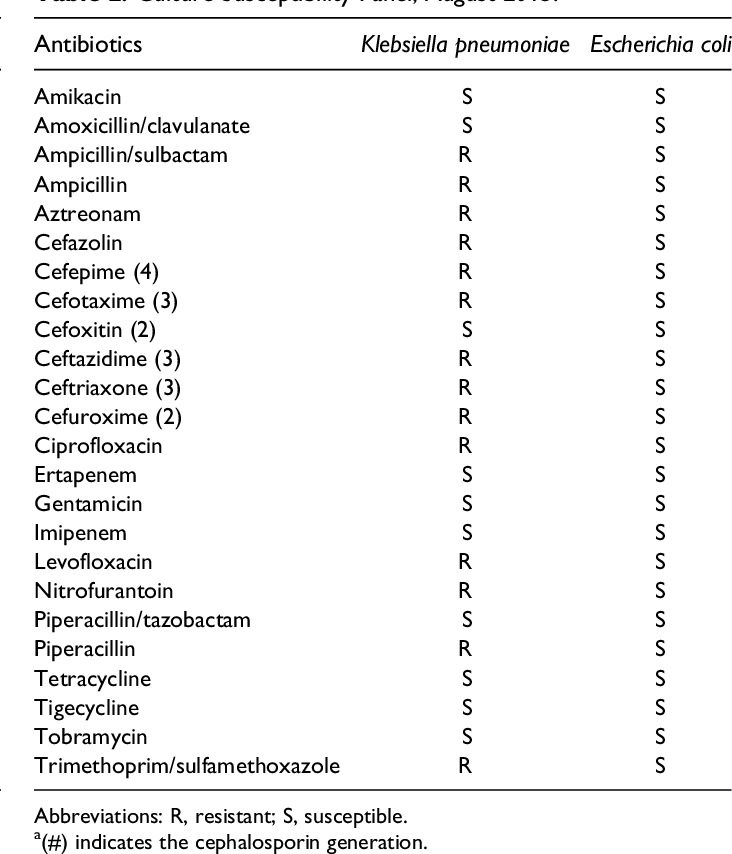
Important Considerations: While doxycycline *can* work against some E. coli strains, resistance is growing. A urine culture and antibiotic sensitivity testing are crucial steps in determining the best course of action. These tests identify the specific bacteria causing the infection and determine which antibiotics will be most effective. Ignoring this and self-medicating can lead to treatment failure and potential complications.
Remember: This information should not replace professional medical advice. A proper diagnosis and treatment plan from a healthcare provider are vital for managing a UTI effectively. Early intervention is key to a quick recovery. Seek immediate medical attention if you experience symptoms of a UTI.
- Doxycycline for E. coli UTI: A Detailed Overview
- Understanding E. coli UTIs and Treatment Options
- Doxycycline’s Mechanism of Action Against E. coli
- Targeting Bacterial Ribosomes
- Broad-Spectrum Activity
- Efficacy and Limitations of Doxycycline for E. coli UTIs
- Considerations and Alternatives: When to Use Doxycycline and When Not To
Doxycycline for E. coli UTI: A Detailed Overview
Doxycycline isn’t the first-line treatment for E. coli UTIs. Doctors typically prescribe antibiotics like nitrofurantoin or trimethoprim-sulfamethoxazole. However, doxycycline can be a viable alternative in specific situations.
Its effectiveness depends on the specific strain of E. coli. Antibiotic susceptibility testing is crucial; this lab test determines which antibiotics will work best against the infecting bacteria. Without this, prescribing doxycycline risks treatment failure.
Doxycycline’s advantage lies in its ability to reach high concentrations in the urinary tract. This makes it effective against some resistant E. coli strains, where other antibiotics fail. However, widespread antibiotic resistance is a growing concern, impacting doxycycline’s efficacy.
Potential side effects include nausea, vomiting, diarrhea, and photosensitivity (sun sensitivity). Patients should inform their doctor about all medications they are currently taking to avoid interactions. Pregnancy and breastfeeding considerations exist; always discuss this with your doctor before taking doxycycline.
The dosage and duration of treatment vary depending on the severity of the infection and individual patient factors. A doctor will determine the appropriate regimen. Never adjust the dosage or stop the medication prematurely without consulting a physician, even if symptoms improve.
While doxycycline can treat E. coli UTIs in certain cases, it’s vital to seek medical attention for diagnosis and treatment. Self-treating a UTI with doxycycline or any antibiotic is dangerous and can lead to complications, including antibiotic resistance.
Understanding E. coli UTIs and Treatment Options
E. coli bacteria cause most urinary tract infections (UTIs). These infections can range from mild bladder infections (cystitis) to more serious kidney infections (pyelonephritis). Early diagnosis and treatment are crucial.
Symptoms of a UTI include:
- A strong, persistent urge to urinate
- Burning sensation during urination
- Passing frequent, small amounts of urine
- Cloudy, dark, bloody, or foul-smelling urine
- Pelvic pain (women)
- Lower back or side pain (kidney infection)
If you experience these symptoms, seek medical attention. A urine test confirms the diagnosis. Your doctor will determine the best treatment based on your specific situation.
Common UTI treatment options include:
- Antibiotics: Doxycycline is one possibility, often prescribed for uncomplicated UTIs. Other antibiotics like nitrofurantoin, trimethoprim-sulfamethoxazole, and ciprofloxacin are also used, with choices depending on the specific bacteria and your medical history. Always complete the full course of antibiotics, even if symptoms improve.
- Increased fluid intake: Drinking plenty of water helps flush out bacteria.
- Over-the-counter pain relievers: Acetaminophen or ibuprofen can help manage pain and fever.
- Cranberry products: While not a substitute for antibiotics, some studies suggest cranberry products may help prevent UTIs.
Prevention strategies include:
- Wiping front to back after urination and bowel movements.
- Drinking plenty of fluids.
- Urinating frequently.
- Emptying your bladder completely.
- Avoiding tight-fitting clothing.
Note: This information is for general knowledge and does not substitute professional medical advice. Always consult a doctor for diagnosis and treatment of UTIs.
Doxycycline’s Mechanism of Action Against E. coli
Doxycycline inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit of E. coli. This binding prevents the attachment of aminoacyl-tRNA to the mRNA-ribosome complex, halting translation. Consequently, the bacterium cannot produce the proteins necessary for growth and survival.
Targeting Bacterial Ribosomes
Specifically, doxycycline interacts with the 16S rRNA within the 30S subunit. This interaction is crucial because it blocks the A site, the ribosomal binding site for aminoacyl-tRNA. This blockage directly prevents the addition of new amino acids to the growing polypeptide chain, ultimately leading to bacterial death.
Broad-Spectrum Activity
This mechanism explains doxycycline’s broad-spectrum activity against a wide range of bacteria, including many strains of E. coli. However, resistance mechanisms, such as ribosomal mutations, can develop, reducing doxycycline’s efficacy in certain bacterial populations.
Efficacy and Limitations of Doxycycline for E. coli UTIs
Doxycycline isn’t the first-line treatment for uncomplicated E. coli UTIs. While it possesses some activity against E. coli, its efficacy is variable and depends heavily on the specific strain’s susceptibility. Fluoroquinolones and trimethoprim-sulfamethoxazole are generally preferred due to their higher success rates and established clinical experience.
Doxycycline’s main limitation lies in its increasing resistance among E. coli isolates. Many studies demonstrate a rise in resistance rates globally. Therefore, relying on doxycycline without prior susceptibility testing increases the risk of treatment failure and potential complications.
Another factor to consider is that doxycycline’s activity against E. coli is primarily bacteriostatic, meaning it inhibits bacterial growth rather than killing the bacteria outright. This can prolong the duration of infection and increase the chance of relapse compared to bactericidal antibiotics.
Furthermore, doxycycline can interact with other medications, potentially causing adverse effects. Patients should always disclose all medications, supplements, and herbal remedies to their doctor before starting doxycycline.
| Factor | Impact on Doxycycline Use for E. coli UTIs |
|---|---|
| Resistance Rates | Increasing, reducing treatment success. |
| Bacteriostatic Action | Slows bacterial growth, increasing relapse risk. |
| Drug Interactions | Potential for adverse effects with other medications. |
| Alternative Treatments | Fluoroquinolones and trimethoprim-sulfamethoxazole are generally preferred. |
In summary, while doxycycline may show some activity against certain E. coli strains, its use for UTIs should be guided by antibiotic susceptibility testing and carefully weighed against the potential drawbacks and availability of more effective alternatives.
Considerations and Alternatives: When to Use Doxycycline and When Not To
Doxycycline isn’t the first-line treatment for E. coli UTIs. Reserve it for specific situations.
Use doxycycline if: You have a penicillin allergy and other alternatives are unsuitable; your doctor confirms E. coli susceptibility to doxycycline; you’ve failed treatment with other antibiotics. Always follow your doctor’s guidance on dosage and duration.
Avoid doxycycline if: You’re pregnant or breastfeeding; you have liver or kidney problems; you’re sensitive to tetracyclines; you’re under eight years old; you’re taking certain medications that interact negatively. These interactions can reduce doxycycline’s effectiveness or cause adverse reactions.
Better alternatives usually include: Nitrofurantoin, trimethoprim-sulfamethoxazole (TMP-SMX), or fosfomycin. These are generally preferred due to lower risk of side effects and better efficacy against common UTI pathogens. Your doctor will determine the best option based on your medical history and test results.
Important Note: Antibiotic resistance is a growing problem. Improper antibiotic use contributes to this. Never self-medicate. Always consult a doctor for diagnosis and treatment of a UTI.
Further testing may be needed: If symptoms persist after treatment, repeat testing might be necessary to identify the causative bacteria and determine antibiotic susceptibility. This ensures appropriate treatment is administered.