Suspect an amoxicillin allergy? First, seek immediate medical attention if you’re experiencing a severe reaction, like difficulty breathing or swelling. This is crucial for your safety.
Amoxicillin allergies manifest differently in individuals. Common symptoms include hives, itching, and rash. Less frequent, but more serious, reactions involve swelling of the face, lips, or tongue (angioedema) and breathing difficulties. Accurate diagnosis is paramount; a doctor will determine the severity and guide you on appropriate management.
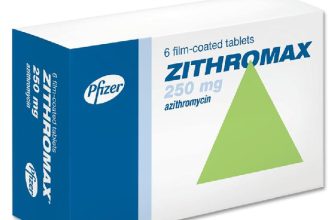
Several factors influence the severity of an allergic reaction. Your medical history, the amoxicillin dosage, and the route of administration (oral vs. injection) all play a role. Knowing these specifics helps your doctor tailor the best treatment plan. Alternatives to amoxicillin exist, such as azithromycin or cefdinir, depending on the infection. Your physician will carefully consider these options based on your individual needs.
Prevention is key. Always inform your doctor and pharmacist about any allergies before taking any medication. Wear a medical alert bracelet or necklace if you have a severe allergy. This precaution ensures swift and appropriate medical response during an emergency.
- Allergy to Amoxicillin: A Comprehensive Guide
- What are the symptoms of an amoxicillin allergy?
- Skin Reactions
- Respiratory Symptoms
- Other Symptoms
- Timing of Symptoms
- Seeking Medical Attention
- How is an amoxicillin allergy diagnosed?
- What are the treatment options for an amoxicillin allergic reaction?
- What are the long-term implications of an amoxicillin allergy?
- Understanding Cross-Reactivity
- Managing Your Allergy
- What alternative antibiotics are available?
- How can I prevent future amoxicillin allergic reactions?
- Understanding Your Reaction
- Alternative Antibiotics
- Emergency Preparedness
- Skin Testing
- Medication Reconciliation
Allergy to Amoxicillin: A Comprehensive Guide
See your doctor immediately if you experience symptoms like hives, swelling, or difficulty breathing after taking amoxicillin. This indicates a potential severe allergic reaction requiring immediate medical attention.
Amoxicillin allergies manifest differently. Some experience mild skin rashes; others face life-threatening anaphylaxis. Knowing your reaction’s severity is crucial for future medical decisions.
Accurate diagnosis relies on a detailed medical history and potentially allergy testing. Your doctor will assess your symptoms and determine the best course of action.
Avoid all penicillin-based antibiotics if you have a confirmed amoxicillin allergy. Penicillins share similar structures, increasing your risk of cross-reactivity.
Alternative antibiotics exist. Your physician will select an appropriate replacement based on your infection and allergy history. This might include macrolides, cephalosporins, or others.
Always inform healthcare providers of your amoxicillin allergy. This prevents accidental exposure and ensures your safety during medical procedures or prescriptions.
Carry an emergency epinephrine auto-injector (like an EpiPen) if you’ve experienced anaphylaxis. This can be life-saving in the event of a future reaction.
| Symptom | Severity | Action |
|---|---|---|
| Skin rash | Mild | Stop taking amoxicillin; consult your doctor. |
| Swelling (face, lips, tongue) | Moderate to Severe | Seek immediate medical attention. |
| Difficulty breathing | Severe | Use epinephrine auto-injector; call emergency services immediately. |
| Wheezing | Moderate to Severe | Seek immediate medical attention. |
Managing your amoxicillin allergy involves careful monitoring, proactive communication with your doctor, and prompt action if symptoms appear. Your health and safety are paramount.
What are the symptoms of an amoxicillin allergy?
Amoxicillin allergies manifest in various ways, ranging from mild to severe. Recognizing these symptoms is crucial for prompt treatment.
Skin Reactions
- Hives (urticaria): Raised, itchy welts on the skin.
- Rash: Red, bumpy, or blotchy skin.
- Itching: Intense skin irritation.
- Angioedema: Swelling of the face, lips, tongue, or throat.
These skin reactions can appear anywhere on the body and may be accompanied by fever.
Respiratory Symptoms
- Wheezing: A whistling sound during breathing.
- Shortness of breath.
- Difficulty breathing.
- Cough.
Respiratory symptoms indicate a more serious allergic reaction and require immediate medical attention.
Other Symptoms
- Nausea
- Vomiting
- Diarrhea
- Anaphylaxis: A severe, life-threatening allergic reaction characterized by sudden drop in blood pressure, rapid heartbeat, dizziness, and loss of consciousness. This necessitates immediate emergency medical care.
Timing of Symptoms
Symptoms can appear within minutes to hours after taking amoxicillin. However, in some cases, a delayed reaction might occur.
Seeking Medical Attention
If you experience any of these symptoms after taking amoxicillin, stop taking the medication immediately and contact a doctor or seek emergency medical assistance.
How is an amoxicillin allergy diagnosed?
A doctor will usually diagnose an amoxicillin allergy based on your medical history and a physical exam. They’ll ask about your symptoms and when they appeared after taking amoxicillin. Be prepared to describe the reaction in detail – including the type of symptoms (rash, swelling, difficulty breathing, etc.), their severity, and how long they lasted.
Skin prick tests or blood tests can sometimes confirm an allergy. A skin prick test involves placing a tiny amount of amoxicillin on your skin and pricking the skin to see if there’s a reaction. Blood tests measure the levels of specific antibodies in your blood that indicate an allergic response to amoxicillin. Note that these tests aren’t always conclusive; a negative result doesn’t guarantee you won’t react, while a positive result confirms sensitivity but not necessarily the severity of a reaction.
Your doctor might also consider other factors, such as your family history of allergies and any previous reactions to penicillin-type antibiotics. This complete picture helps determine the best course of action. Remember to always inform your doctor of all medications and supplements you’re taking.
Accurate diagnosis is crucial for safe treatment. If you suspect an amoxicillin allergy, seek medical attention immediately. Your doctor will guide you on the appropriate management and alternative medications.
What are the treatment options for an amoxicillin allergic reaction?
Treatment depends entirely on the severity of your reaction. Mild reactions usually require only supportive care.
- Mild reactions (hives, itching): Over-the-counter antihistamines like diphenhydramine (Benadryl) can effectively relieve symptoms. Ensure you follow the dosage instructions on the packaging.
- Moderate reactions (swelling, difficulty breathing): Seek immediate medical attention. Epinephrine (adrenaline) is often administered to counteract the allergic response. This might involve an injection or nebulizer treatment, depending on the situation. Further treatment may include corticosteroids to reduce inflammation.
- Severe reactions (anaphylaxis): This is a life-threatening emergency. Call emergency services immediately. Treatment includes epinephrine injection, oxygen therapy, intravenous fluids, and potentially hospitalization for monitoring and further treatment. You’ll likely require an EpiPen or similar auto-injector for future use.
Following an allergic reaction to amoxicillin, your doctor will likely recommend alternative antibiotics. They will consider your specific needs and the type of infection you are treating to select a safe and appropriate alternative. Common alternatives include:
- Cephalosporins (though cross-reactivity is possible, so discuss this with your doctor)
- Macrolides (e.g., azithromycin, erythromycin)
- Tetracyclines
- Clindamycin
Always inform your doctor and pharmacist of any known allergies before starting any new medication. Carry an allergy alert bracelet or card to inform medical personnel in case of an emergency.
What are the long-term implications of an amoxicillin allergy?
An amoxicillin allergy doesn’t automatically predict future reactions to all antibiotics. However, it increases your risk of developing allergies to other beta-lactam antibiotics, like penicillin, cephalosporins (such as cefixime and ceftriaxone), and carbapenems. This cross-reactivity varies; some individuals react to all, while others tolerate some. Always inform healthcare providers of your amoxicillin allergy to ensure appropriate medication choices.
Understanding Cross-Reactivity
The degree of cross-reactivity depends on the specific allergy’s severity and the shared chemical structure of the antibiotics. Mild amoxicillin reactions might not predict reactions to all beta-lactams. Severe reactions, like anaphylaxis, significantly increase the risk of serious reactions to similar antibiotics. Your doctor can assess your risk and recommend suitable alternatives.
Managing Your Allergy
Carry an allergy alert bracelet or card. This provides crucial information to emergency responders in case of a reaction. Maintain a detailed medical record that includes the type of reaction and the specific antibiotic causing it. This allows healthcare providers to make informed decisions about treatment in the future. Openly discuss your allergy with all healthcare providers involved in your care.
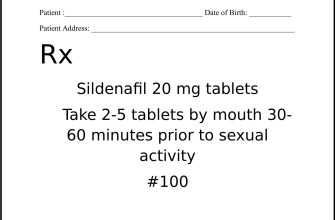
What alternative antibiotics are available?
If you’re allergic to amoxicillin, your doctor will consider your specific needs and the type of infection you have before prescribing an alternative. Common alternatives include cephalosporins like cefalexin or cefuroxime, which are structurally related to penicillins but may be tolerated by those with penicillin allergies. However, cross-reactivity is possible, so careful consideration is required.
Macrolides, such as azithromycin or erythromycin, offer another option. These are effective against many common bacterial infections, but may have longer treatment durations. They’re often prescribed for respiratory infections.
Tetracyclines, including doxycycline and minocycline, provide broad-spectrum coverage and are frequently used for various infections, especially those affecting the skin or respiratory tract. Note that tetracyclines have age restrictions and potential side effects.
For serious infections, your doctor may opt for a fluoroquinolone antibiotic like ciprofloxacin or levofloxacin. These are powerful drugs, but potential side effects must be discussed.
Finally, your doctor might choose a different antibiotic class entirely, depending on the infection and your specific allergy. This may involve a less common antibiotic, tailored to your condition. Always discuss potential alternatives and risks with your physician.
How can I prevent future amoxicillin allergic reactions?
First, always inform every healthcare provider about your amoxicillin allergy. This includes doctors, dentists, and nurses. Wear a medical alert bracelet or necklace clearly stating your allergy.
Understanding Your Reaction
Knowing the type of reaction you experienced is crucial. A mild rash differs significantly from anaphylaxis. Document your symptoms precisely. This detailed information helps your doctor determine the best course of action for future treatments.
Alternative Antibiotics
Discuss alternative antibiotics with your doctor. Many options exist, and your physician can choose one appropriate for your condition and less likely to trigger a reaction. They will consider the severity of your infection and your individual health history.
Emergency Preparedness
If you’ve experienced a severe reaction like anaphylaxis, carry an epinephrine auto-injector (like an EpiPen) at all times. Learn how to use it correctly through proper training provided by your physician or pharmacist. Regularly check the expiration date and replace it as needed.
Skin Testing
Your doctor might recommend allergy testing to determine the specific component of amoxicillin causing your reaction. This can help identify safer alternatives or predict potential cross-reactivity with other medications.
Medication Reconciliation
Maintain a detailed list of all medications, supplements, and herbal remedies you take. Provide this list to any healthcare provider before starting any new treatment to prevent interactions and unexpected reactions. This proactive approach minimizes risks.