Ampicillin serves as a reliable antibiotic for treating a variety of bacterial infections. It effectively combats infections such as pneumonia, meningitis, and urinary tract infections. When prescribed, ensure adherence to the dosage schedule provided by your healthcare professional to maximize its efficacy.
This antibiotic operates by inhibiting bacterial cell wall synthesis, leading to the disruption of vital functions in susceptible bacteria. It is part of the penicillin family and covers a broad spectrum of gram-positive and some gram-negative bacteria. If you or your doctor suspect a bacterial infection, discuss the benefits of ampicillin along with potential side effects.
While ampicillin can be beneficial, monitoring for allergic reactions is crucial. If you experience symptoms like rash, itching, or difficulty breathing, seek medical attention promptly. Maintaining open communication with your healthcare provider about your medical history can help ensure a safe treatment plan.
Consider ampicillin’s interaction with other medications you might be taking. Some antibiotics might reduce the effectiveness of other drugs. Always inform your doctor about all medications and supplements in use to avoid complications. Regular follow-ups might be necessary to evaluate treatment progress and manage any side effects effectively.
Antibiotics Ampicillin: A Detailed Overview
Ampicillin acts as a broad-spectrum antibiotic effective against numerous bacterial infections. It targets gram-positive and certain gram-negative bacteria, making it suitable for treating conditions like respiratory tract infections, urinary tract infections, and meningitis.
This medication works by inhibiting the synthesis of bacterial cell walls, leading to cell lysis and death. Administering ampicillin intravenously or orally ensures absorption that can be tailored based on the severity of the infection.
Dosage typically starts at 250 mg to 500 mg every 6 hours for adults. Adjustments depend on the specific infection and patient response. Monitoring renal function is necessary, as compromised kidney function may require lower doses.
Ampicillin is generally well-tolerated, though side effects can occur. Common reactions include gastrointestinal disturbances, such as diarrhea and nausea. Allergic reactions, while rare, may manifest as rash or anaphylaxis. Prompt attention to any severe side effects is crucial.
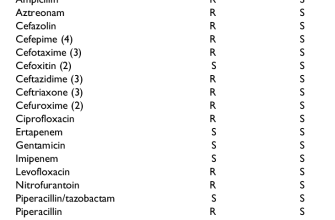
Be aware that resistance has emerged in certain bacterial strains, limiting ampicillin’s effectiveness. Sensitivity testing is advisable to ensure appropriate use and avoid unnecessary broad-spectrum therapy.
In combination with other antibiotics, ampicillin can enhance treatment for infections where multiple pathogens are involved. Discuss options with a healthcare provider to determine the best regimen based on individual circumstances.
Patients should complete the full course of treatment, even if symptoms improve. This practice minimizes the risk of developing resistance and ensures complete eradication of the infection.
When storing ampicillin capsules or tablets, keep them in a cool, dry place away from light. Liquid formulations require refrigeration and should be discarded after 14 days if not used.
Consult healthcare professionals for guidance on potential interactions with other medications, especially with anticoagulants and some oral contraceptives. Regular check-ups can help monitor the treatment’s progress and ensure safety.
Clinical Uses and Effectiveness of Ampicillin
Ampicillin targets a range of bacterial infections, establishing itself as a first-line antibiotic in various clinical scenarios. It effectively combats gram-positive and some gram-negative bacteria, making it suitable for treating respiratory, gastrointestinal, and urinary tract infections.
- Respiratory Infections: Ampicillin is prescribed for pneumonia and bronchiolitis caused by susceptible strains, particularly in hospitalized patients.
- Gastrointestinal Tract Infections: This antibiotic is beneficial for treating infections resulting from Escherichia coli and Salmonella species.
- Urinary Tract Infections: Ampicillin proves effective against uncomplicated UTIs, especially in pregnant women.
- Meningitis: In pediatric settings, ampicillin is part of the treatment regimen for certain types of bacterial meningitis.
- Endocarditis: Used in prophylactic settings, ampicillin prevents endocarditis in patients undergoing dental procedures who are at risk.
The dosing of ampicillin varies based on the infection type and patient demographics. For adults, the typical dosage ranges from 250 mg to 500 mg every six hours. For children, the dosage is calculated based on weight, which ensures proper efficacy.
Monitoring for allergic reactions and gastrointestinal side effects is crucial. Healthcare providers usually recommend taking ampicillin on an empty stomach to enhance absorption, allowing for maximum therapeutic benefit.
Ampicillin consistently shows high sensitivity in treating penicillin-sensitive strains. However, resistance remains a concern. Regular susceptibility testing is advisable to confirm effectiveness against the specific pathogens involved in an infection.
In summary, ampicillin serves as a reliable antibiotic for managing various infections, with careful attention to dosing, monitoring, and resistance patterns ensuring optimal clinical outcomes.
Administration and Dosage Guidelines for Ampicillin
Ampicillin is typically administered intravenously or intramuscularly for optimal absorption and effectiveness. The usual loading dose for adults ranges from 1 to 2 grams, given every 6 to 8 hours. After the initial dose, maintenance dosages can be adjusted depending on the severity of the infection and the patient’s response.
For adult respiratory tract infections, the recommended dosage is 500 mg to 1 gram every 6 hours. In cases of more severe infections, this can be increased to 2 grams every 6 hours. For urinary tract infections, prescribe 500 mg every 6 hours.
In pediatric patients, the dosing typically is based on body weight. A standard recommendation is 50 to 100 mg/kg/day, divided into doses taken every 6 to 8 hours. For severe infections, this may increase to 200 mg/kg/day.
Adjustments are necessary for patients with renal impairment. Monitor kidney function closely. For patients on dialysis, additional doses may be required after the procedure.
Monitor for signs of allergic reactions or gastrointestinal side effects. If these occur, discontinue the medication and consult healthcare providers. Always consider potential interactions with other medications.
Consult local guidelines and consider individual patient factors such as age, weight, and renal function when determining final dosages. Regular follow-up is recommended to assess treatment effectiveness and adjust as needed.
Side Effects and Recommendations for Ampicillin Use
Monitor for allergic reactions when taking ampicillin. Symptoms may include rash, itching, or swelling, particularly of the face, tongue, or throat. If any of these occur, seek immediate medical attention.
Gastrointestinal issues such as diarrhea, nausea, or vomiting often arise with ampicillin. Eating smaller, more frequent meals can help minimize discomfort. If diarrhea becomes severe or persists, contact a healthcare provider, as it may indicate a more serious condition.
Hydration and Dietary Considerations
Stay well-hydrated while using ampicillin. Drinking plenty of water supports kidney function, aiding in the elimination of the medication. It’s advisable to avoid dairy products close to the time of taking the antibiotic, as they can interfere with absorption. Instead, opt for non-dairy sources of calcium during treatment.
Completing the Course
Always complete the prescribed course of ampicillin, even if symptoms improve before finishing. Stopping too early may lead to antibiotic resistance or recurrence of the infection. Consistently follow the dosing schedule without skipping doses.