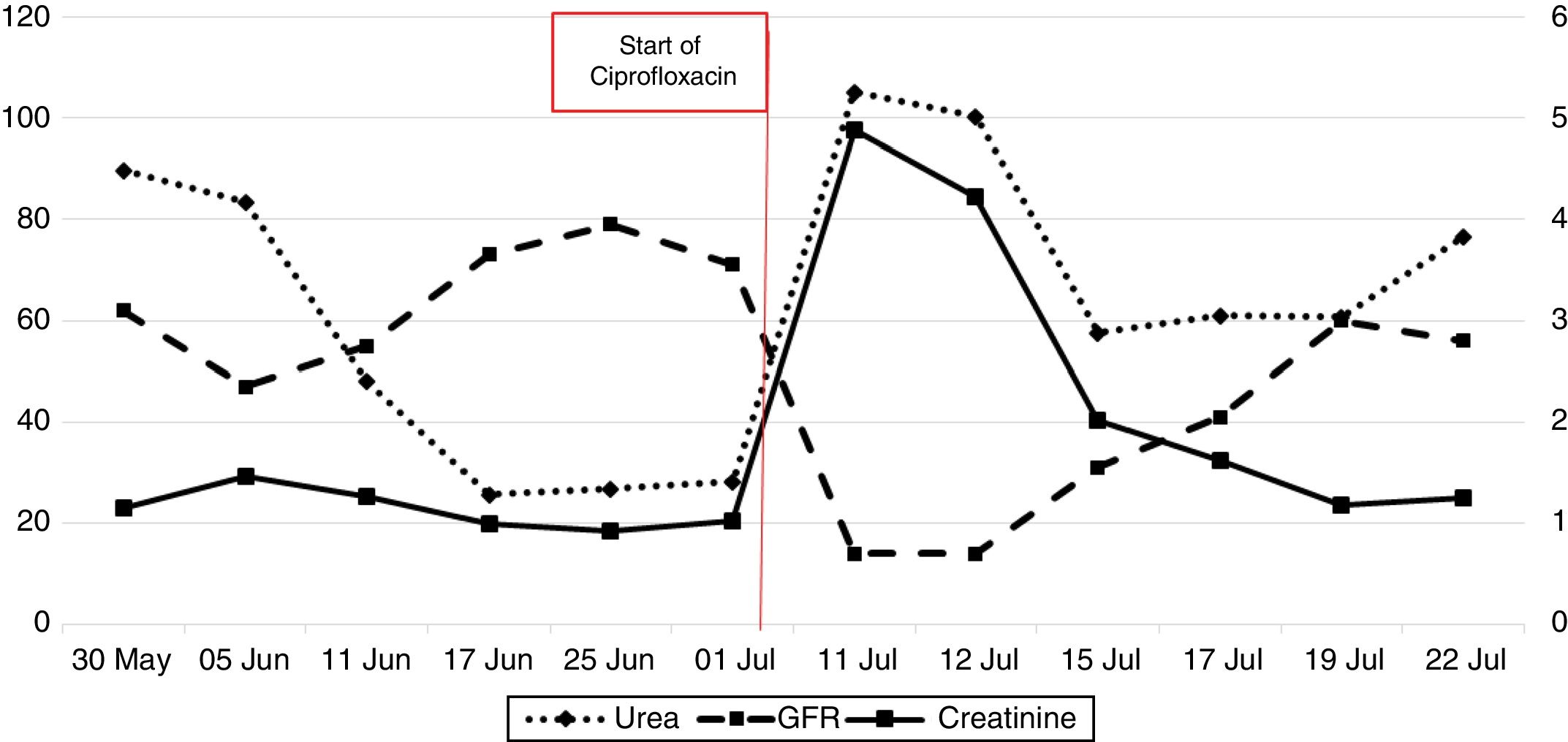
Monitor creatinine levels closely before, during, and after Ciprofloxacin treatment, especially in patients with pre-existing kidney conditions. This proactive approach helps prevent potential complications.
Patients with impaired renal function may require dosage adjustments. Consult the prescribing information for specific guidelines based on creatinine clearance. Lower doses are generally recommended to minimize the risk of adverse reactions.
Hydration plays a critical role. Encourage adequate fluid intake to promote Ciprofloxacin excretion and reduce nephrotoxicity risk. This simple measure can significantly improve patient outcomes.
Regularly assess renal function parameters, such as serum creatinine and estimated glomerular filtration rate (eGFR). These objective measurements provide valuable insights into kidney health and help guide treatment decisions. Prompt identification of any deterioration allows for timely intervention.
Consider alternative antibiotics if the patient’s renal function is severely compromised. Not all antibiotics interact with the kidneys in the same way, and a different medication might be a safer option. A thorough review of patient history and current health status is paramount.
- Cipro and Renal Function: A Detailed Overview
- Ciprofloxacin’s Mechanism of Excretion
- Renal Impairment and Ciprofloxacin Dosage Adjustment
- Monitoring Renal Function During Ciprofloxacin Treatment
- Frequency of Monitoring
- Interpreting Results
- Additional Considerations
- Specific Renal Side Effects Associated with Ciprofloxacin
- Ciprofloxacin and Acute Kidney Injury (AKI): Risk Factors and Prevention
- Alternative Antibiotics for Patients with Renal Dysfunction
- Alternative Antibiotics Based on Infection Type
- Monitoring Renal Function During Treatment
- Patient Counseling and Medication Adherence with Ciprofloxacin
- Understanding Potential Side Effects
- Optimizing Adherence
- Renal Function Monitoring
- Hydration & Diet
- Follow-up
- Long-Term Renal Effects of Ciprofloxacin Use
Cipro and Renal Function: A Detailed Overview
Ciprofloxacin, or Cipro, is excreted primarily by the kidneys. This means reduced kidney function directly impacts how your body processes the drug. Monitor creatinine clearance (CrCl) before prescribing; this provides a reliable estimate of your patient’s kidney function.
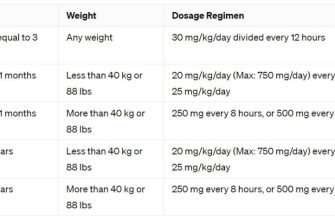
Dosage Adjustments: For patients with mild to moderate renal impairment (CrCl 30-80 mL/min), reduce the Cipro dosage. Consult the prescribing information for specific recommendations. For patients with severe renal impairment (CrCl <30 mL/min), further dosage reduction or alternative antibiotic selection is often necessary.
Creatinine and BUN levels: Regularly monitor serum creatinine and blood urea nitrogen (BUN) levels during Cipro treatment, particularly in patients with pre-existing renal issues. Significant elevations suggest potential nephrotoxicity.
Risk Factors: Patients with pre-existing kidney disease, older adults (due to age-related decline in kidney function), and those taking nephrotoxic medications concurrently are at increased risk of Cipro-induced nephrotoxicity.
Adverse Effects: While rare, Cipro can cause acute kidney injury (AKI). Symptoms may include decreased urine output, edema, fatigue, and nausea. Promptly discontinue Cipro and initiate supportive care if AKI is suspected.
Alternative Antibiotics: Consider alternative antibiotics for patients with severe renal impairment or a history of Cipro-induced nephrotoxicity. Levofloxacin presents similar renal excretion characteristics and requires similar dosage adjustments.
Hydration: Adequate hydration helps facilitate Cipro excretion. Encourage patients to maintain sufficient fluid intake during treatment.
Monitoring: Closely monitor patients at high risk for renal complications. Regular assessments of renal function are crucial for safe and effective Cipro administration.
Ciprofloxacin’s Mechanism of Excretion
Ciprofloxacin, primarily, exits the body through the kidneys. About 50% of an administered dose is excreted unchanged in the urine within 24 hours.
Renal tubular secretion plays a significant role in this process. This active transport mechanism moves the drug from the bloodstream into the renal tubules, facilitating its elimination.
Glomerular filtration also contributes to ciprofloxacin’s removal. This passive process filters the drug from the blood into the glomerular filtrate.
A smaller portion (about 30%) is metabolized in the liver, with metabolites also being excreted via the kidneys.
Factors like age, renal function, and concomitant medications can influence the rate of excretion. Reduced kidney function significantly slows this process, potentially leading to drug accumulation.
Dosage adjustments are frequently necessary for patients with impaired renal function to prevent toxicity. Careful monitoring of serum creatinine levels is crucial in these cases.
Patients with severe renal insufficiency may require alternative antibiotics. Consult your physician or pharmacist for appropriate dosage adjustments or alternative therapies based on individual renal function.
Renal Impairment and Ciprofloxacin Dosage Adjustment
Ciprofloxacin dosage requires adjustment for patients with impaired renal function. This is because the kidneys are the primary route of elimination for this medication. Failure to adjust the dose can lead to drug accumulation and increased risk of adverse effects.
Dosage adjustments are typically based on creatinine clearance (CrCl), a measure of kidney function. You should consult a creatinine clearance calculator or your physician to determine the appropriate CrCl value for your patient. Here’s a general guideline, but always refer to the most up-to-date prescribing information:
| Creatinine Clearance (CrCl) mL/min | Ciprofloxacin Dosage Adjustment |
|---|---|
| ≥50 | Standard dose |
| 30-49 | Reduce dose by 50% |
| <30 | Significant dose reduction or alternative therapy may be necessary. Consult a nephrologist. |
For patients undergoing hemodialysis, a supplemental dose may be needed after each dialysis session. The specific timing and amount should be determined by a healthcare professional familiar with your patient’s condition.
Regular monitoring of renal function and serum ciprofloxacin levels is recommended, particularly in patients with severe renal impairment. Closely observe your patient for signs of toxicity, such as nausea, vomiting, diarrhea, or confusion. Report any adverse reactions to the prescribing physician immediately.
Remember, this information is for guidance only and does not replace individual clinical judgment and consultation with prescribing information. Always tailor treatment to the specific needs of your patient. The prescribing information should be the ultimate authority for dosage recommendations.
Monitoring Renal Function During Ciprofloxacin Treatment
Regularly assess renal function before initiating Ciprofloxacin therapy and throughout treatment. Baseline serum creatinine and estimated glomerular filtration rate (eGFR) measurements are crucial.
Frequency of Monitoring
For patients with normal baseline renal function, monitor serum creatinine and eGFR at least once during treatment, particularly in those receiving prolonged courses (more than 10 days). For patients with pre-existing renal impairment (eGFR <60 mL/min/1.73m²), more frequent monitoring, such as weekly checks, is necessary. Adjust dosage as per renal function guidelines. Consider monitoring for signs of nephrotoxicity such as increased serum creatinine, decreased eGFR, and proteinuria.
Interpreting Results
A significant increase in serum creatinine (greater than 25% above baseline) or a substantial decrease in eGFR warrants immediate attention. Clinicians should carefully weigh the risks and benefits of continuing Ciprofloxacin therapy, considering alternative treatments when appropriate. Promptly report significant changes to the treating physician.
Additional Considerations
Age: Older adults are more susceptible to Ciprofloxacin-induced nephrotoxicity due to age-related decline in renal function. Concomitant Medications: Certain medications, like NSAIDs, can increase the risk of renal damage when used with Ciprofloxacin. Underlying Conditions: Patients with pre-existing kidney disease, heart failure, or dehydration are at higher risk. Closely monitor these individuals.
Specific Renal Side Effects Associated with Ciprofloxacin
Ciprofloxacin, while generally well-tolerated, can cause several specific renal side effects. Acute kidney injury (AKI) is a known risk, manifesting as decreased urine output and elevated creatinine levels. This typically occurs within days of starting the medication, though delayed onset is possible. Proper hydration is crucial to mitigate this risk.
Interstitial nephritis, an inflammation of the kidney tissue, is another potential side effect. Symptoms include fever, rash, and flank pain, often accompanied by worsening kidney function. Immediate medical attention is necessary if these symptoms appear.
Crystalluria, the presence of crystals in the urine, is a potential complication, particularly with high doses or inadequate hydration. While often asymptomatic, it can lead to kidney stones in susceptible individuals. Maintaining adequate fluid intake helps prevent crystal formation.
Monitoring creatinine and blood urea nitrogen (BUN) levels regularly during treatment, especially in patients with pre-existing kidney disease or those at high risk, is recommended. Adjusting dosage or choosing alternative antibiotics might be necessary depending on renal function. Patients should promptly report any unusual symptoms, such as changes in urination or pain in their lower back.
While rare, tubulointerstitial nephritis and papillary necrosis are severe renal complications linked to ciprofloxacin use. These conditions require immediate medical intervention. Careful patient selection and monitoring are key to minimizing the risk of such severe events.
Ciprofloxacin and Acute Kidney Injury (AKI): Risk Factors and Prevention
Monitor creatinine levels closely, especially in patients with pre-existing renal impairment.
Several factors increase the risk of Ciprofloxacin-induced AKI. Let’s examine these:
- Pre-existing Renal Dysfunction: Patients with impaired kidney function are significantly more vulnerable. Higher baseline creatinine levels directly correlate with increased AKI risk.
- Age: Older adults, generally over 65, exhibit higher susceptibility due to age-related decline in renal function.
- Dehydration: Inadequate fluid intake concentrates Ciprofloxacin in the kidneys, raising the risk of nephrotoxicity.
- Concurrent Medications: Concomitant use of nephrotoxic drugs, such as NSAIDs or aminoglycosides, dramatically increases the likelihood of AKI.
- High Doses and Prolonged Treatment: Extended treatment durations and higher Ciprofloxacin dosages amplify the risk of kidney damage.
- Heart Failure: Patients with heart failure often have reduced renal perfusion, making them more susceptible to Ciprofloxacin-induced AKI.
Prevention strategies focus on mitigating these risk factors:
- Careful Patient Selection: Assess renal function before prescribing Ciprofloxacin. Consider alternative antibiotics if renal impairment is severe.
- Dose Adjustment: Reduce dosage or extend dosing intervals for patients with compromised renal function, following established guidelines.
- Hydration: Encourage adequate fluid intake to maintain sufficient renal perfusion and reduce Ciprofloxacin concentration in the kidneys.
- Medication Review: Thoroughly review the patient’s medication list to identify potential drug interactions that increase AKI risk. Consider alternatives when possible.
- Close Monitoring: Regularly monitor serum creatinine levels, especially during and after Ciprofloxacin treatment. Promptly adjust therapy if creatinine elevation occurs.
Remember: This information is for educational purposes and does not substitute professional medical advice. Always consult with a healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Alternative Antibiotics for Patients with Renal Dysfunction
For patients with impaired kidney function needing antibiotic treatment, careful selection is crucial. Ciprofloxacin, due to its renal excretion, requires dose adjustment or alternative choices. Consider these alternatives:
Alternative Antibiotics Based on Infection Type
For uncomplicated urinary tract infections (UTIs): Nitrofurantoin is often preferred, as it’s primarily eliminated through the urine and requires minimal dosage adjustment in mild to moderate renal impairment. Fosfomycin, another option, is single-dose and excreted unchanged, making it suitable for patients with renal dysfunction. However, always check the specific prescribing information for your patient’s creatinine clearance.
For complicated UTIs or other infections: Aztreonam, a monobactam, is renally cleared but usually requires less dosage adjustment compared to Ciprofloxacin. Certain cephalosporins, like cefazolin, display similar behavior. Aminoglycosides (gentamicin, tobramycin) need significant dose adjustments due to their renal elimination; accurate monitoring of serum drug levels is paramount. Consider carbapenems (imipenem, meropenem) for severe infections; however, they too may require dose modifications dependent on renal function. Always consult a pharmacist or infectious disease specialist for individualized dosage regimens.
Monitoring Renal Function During Treatment
Regularly monitor serum creatinine and estimated glomerular filtration rate (eGFR) during antibiotic treatment, especially with drugs exhibiting significant renal clearance. Adjust the dose or consider alternative medication as renal function changes. Closely follow the patient’s clinical response to the chosen antibiotic.
Patient Counseling and Medication Adherence with Ciprofloxacin
Clearly explain the importance of taking Ciprofloxacin exactly as prescribed, emphasizing the need to complete the entire course of treatment, even if symptoms improve early. This prevents antibiotic resistance and ensures optimal treatment.
Understanding Potential Side Effects
Discuss common side effects like nausea, diarrhea, and abdominal pain. Explain less common but potentially serious side effects, such as tendon rupture, peripheral neuropathy, and worsening renal function. Stress the importance of reporting any unusual symptoms to their physician immediately.
- Provide patients with a written list of potential side effects and when to seek medical attention.
- Encourage patients to keep a symptom diary to track any adverse events.
Optimizing Adherence
- Use clear, simple language, avoiding medical jargon.
- Verify patient understanding through open-ended questions, not just yes/no questions.
- Provide practical strategies for remembering to take medication, such as using a pill organizer or setting medication reminders on their phone.
- Address any concerns or misconceptions the patient may have regarding Ciprofloxacin or antibiotic treatment.
- Explore any barriers to medication adherence, such as cost, access, or other medications they are taking. Work with the patient to find solutions.
Renal Function Monitoring
Explain the potential impact of Ciprofloxacin on kidney function, especially in patients with pre-existing renal impairment or those taking other nephrotoxic medications. Highlight the need for regular monitoring of kidney function during and after treatment. Emphasize scheduled follow-up appointments to check blood and urine tests.
Hydration & Diet
- Instruct patients to drink plenty of fluids to aid in the excretion of the medication.
- Recommend a balanced diet to support overall health and minimize potential side effects.
Follow-up
Schedule a follow-up appointment to assess the patient’s response to treatment and monitor for any adverse effects. Address any remaining questions or concerns.
Long-Term Renal Effects of Ciprofloxacin Use
While Ciprofloxacin generally boasts a good safety profile, long-term use carries potential risks to kidney health. Studies show a correlation between prolonged Ciprofloxacin use and a slightly increased risk of chronic kidney disease (CKD), particularly in individuals with pre-existing renal impairment.
This increased risk isn’t massive, but it’s significant enough to warrant caution. Factors like dosage, duration of treatment, and individual patient health significantly influence this risk. Older adults and those with existing kidney problems are more vulnerable.
Specifically, some studies have linked long-term Ciprofloxacin use to interstitial nephritis, a form of kidney inflammation. This can lead to reduced kidney function and, in severe cases, kidney failure. However, this complication is relatively rare.
Regular monitoring of kidney function, including creatinine levels and estimated glomerular filtration rate (eGFR), is recommended for patients on long-term Ciprofloxacin therapy. Your doctor should adjust your dosage or consider alternative antibiotics if your kidney function deteriorates.
Hydration is crucial during Ciprofloxacin treatment to support kidney function. Adequate fluid intake helps flush out the medication and reduces the strain on your kidneys. Consult your doctor or pharmacist regarding safe hydration practices.
Always inform your healthcare provider about your complete medical history, including any pre-existing kidney conditions, before starting Ciprofloxacin treatment. Open communication facilitates informed decision-making and promotes your health.