Ciprofloxacin (Cipro) and metronidazole (Flagyl) are often prescribed together for specific infections, primarily those involving both aerobic and anaerobic bacteria. This combination targets a broader spectrum of pathogens, increasing the likelihood of successful treatment.
Doctors frequently prescribe this dual therapy for serious intra-abdominal infections, pelvic inflammatory disease, and certain types of bacterial vaginosis. The decision to use Cipro and Flagyl rests on a precise diagnosis, considering the likely bacteria involved and the patient’s overall health. Always follow your physician’s instructions carefully.
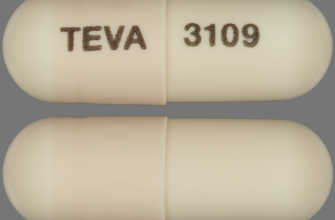
Remember: Cipro and Flagyl have different mechanisms of action and potential side effects. Cipro is a fluoroquinolone antibiotic; Flagyl is a nitroimidazole. Potential side effects, such as nausea, diarrhea, and allergic reactions, vary between individuals and should be discussed with your doctor. Do not stop taking these medications without consulting your healthcare provider.
Seeking clarification on your prescription from a qualified medical professional is paramount. They can assess your specific condition and determine if this antibiotic combination is appropriate for you and adjust the dosage as necessary. Your health and safety are a priority, and informed decision-making is crucial.
- Ciprofloxacin vs. Metronidazole: A Comparative Overview
- Spectrum of Activity
- Administration and Side Effects
- Drug Interactions
- Conclusion
- Ciprofloxacin (Cipro) Mechanism of Action
- Topoisomerase Inhibition: A Closer Look
- Metronidazole (Flagyl) Mechanism of Action
- Specific Targets
- Clinical Implications
- Spectrum of Activity: Cipro vs. Flagyl
- Common Uses and Indications for Cipro and Flagyl
- Ciprofloxacin Treatment Targets
- Metronidazole’s Applications
- Important Note:
- Potential Drug Interactions Between Cipro and Flagyl
- Considerations for Concurrent Use or Sequential Treatment
- Concurrent Use: Potential Interactions
- Sequential Treatment: Strategies and Timing
- Specific Recommendations
- Alternative Treatments
Ciprofloxacin vs. Metronidazole: A Comparative Overview
Ciprofloxacin and metronidazole treat bacterial infections, but target different types of bacteria. Ciprofloxacin, a fluoroquinolone antibiotic, combats gram-negative and some gram-positive bacteria. Metronidazole, a nitroimidazole, effectively targets anaerobic bacteria and some protozoa. The choice depends entirely on the infection’s cause.
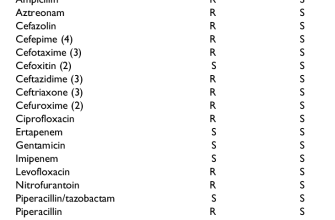
Spectrum of Activity
Ciprofloxacin’s broader spectrum includes E. coli, Salmonella, and Pseudomonas, while metronidazole excels against Clostridium difficile, Bacteroides fragilis, and Trichomonas vaginalis. Doctors consider the specific pathogen when prescribing.
Administration and Side Effects
Both are available orally and intravenously. Common Ciprofloxacin side effects include nausea, diarrhea, and tendon inflammation. Metronidazole’s side effects may include metallic taste, nausea, and vomiting. Always discuss potential interactions with your doctor before starting treatment.
Drug Interactions
Ciprofloxacin interacts with antacids and certain medications affecting the central nervous system. Metronidazole interacts with alcohol and anticoagulants. Thorough medical history is vital for safe prescription.
Conclusion
Ciprofloxacin and metronidazole offer distinct advantages depending on the infection. One isn’t inherently “better” than the other; a physician’s diagnosis guides the appropriate choice. Always follow prescribed dosages and seek medical advice if you experience adverse reactions.
Ciprofloxacin (Cipro) Mechanism of Action
Ciprofloxacin targets bacterial DNA replication. It achieves this by inhibiting bacterial topoisomerase II (DNA gyrase) and topoisomerase IV. These enzymes are crucial for unwinding and separating DNA strands, processes necessary for DNA replication and cell division. By blocking these enzymes, Ciprofloxacin prevents bacteria from copying their genetic material, halting their growth and ultimately leading to their death.
Topoisomerase Inhibition: A Closer Look
Specifically, Ciprofloxacin binds to the topoisomerase-DNA complex, stabilizing it. This prevents the enzyme from releasing the DNA, effectively trapping the enzyme and blocking DNA replication. The bacterial cell can no longer divide or repair its DNA, resulting in bacterial cell death. This mechanism is particularly effective against Gram-negative bacteria, which often possess high levels of topoisomerase II and IV. The drug’s efficacy varies depending on the specific bacterial species and its susceptibility to Ciprofloxacin.
Therefore, Ciprofloxacin’s mechanism relies on precise interaction with bacterial enzymes, leaving human DNA largely unaffected. This selective targeting is key to its antimicrobial activity and explains its efficacy against a broad range of bacterial infections.
Metronidazole (Flagyl) Mechanism of Action
Metronidazole targets anaerobic bacteria and some protozoa by interfering with their DNA. It enters the microorganism’s cell and is reduced by ferredoxin, a bacterial electron carrier. This reduction activates metronidazole, forming a cytotoxic nitro radical anion. This reactive species damages DNA by binding to its helix and disrupting its structure, preventing DNA replication and repair. The damaged DNA leads to cell death.
Specific Targets
Metronidazole’s action is selective because only anaerobic microorganisms and some protozoa possess the required ferredoxin for reduction and activation. Aerobic bacteria lack the reducing environment necessary for this process. Consequently, metronidazole primarily affects organisms living in low-oxygen environments.
Clinical Implications
Understanding this mechanism helps explain its efficacy against various infections, including those caused by Clostridium difficile, Bacteroides species, and Trichomonas vaginalis. However, resistance can develop due to mutations affecting ferredoxin or DNA repair mechanisms.
Spectrum of Activity: Cipro vs. Flagyl
Ciprofloxacin (Cipro) and Metronidazole (Flagyl) target different bacterial groups. Cipro, a fluoroquinolone, excels against gram-negative bacteria like E. coli, Salmonella, and Pseudomonas. Flagyl, a nitroimidazole, is potent against anaerobic bacteria and some protozoa.
Consider this simplified comparison:
| Antibiotic | Gram-positive Bacteria | Gram-negative Bacteria | Anaerobic Bacteria | Protozoa |
|---|---|---|---|---|
| Ciprofloxacin (Cipro) | Limited activity | High activity | Moderate activity against some species | No activity |
| Metronidazole (Flagyl) | Limited activity | Limited activity | High activity | High activity against certain species (e.g., Trichomonas vaginalis, Entamoeba histolytica) |
This table highlights key differences. Cipro’s strength lies in its gram-negative coverage, while Flagyl’s effectiveness centers on anaerobic bacteria and specific protozoa. Always consult a medical professional for accurate diagnosis and treatment. Antibiotic resistance is a serious concern; proper use is critical.
Common Uses and Indications for Cipro and Flagyl
Ciprofloxacin (Cipro) and Metronidazole (Flagyl) treat different bacterial infections. Cipro targets gram-negative bacteria, making it effective against urinary tract infections (UTIs), pneumonia, and some types of diarrhea. It also finds use in treating skin infections and bone and joint infections. Doctors prescribe Cipro for its ability to penetrate tissues well, achieving therapeutic levels in various locations in the body.
Ciprofloxacin Treatment Targets
Common bacterial targets for Ciprofloxacin include E. coli, Pseudomonas aeruginosa, Klebsiella pneumoniae, and Salmonella species.
Metronidazole’s Applications
Flagyl, conversely, tackles anaerobic bacteria and some parasites. It’s frequently prescribed for bacterial vaginosis, pelvic inflammatory disease (PID), and intra-abdominal infections. Flagyl also treats infections caused by Clostridium difficile, a bacterium responsible for antibiotic-associated diarrhea. It’s also effective against certain parasitic infections like giardiasis and trichomoniasis.
Important Note:
Both Cipro and Flagyl require a doctor’s prescription. Individual dosages and treatment durations vary considerably depending on the specific infection, patient factors, and the prescribing physician’s judgment. Always follow your doctor’s instructions carefully and report any adverse reactions immediately. These medications can have side effects, and self-medication is dangerous.
Potential Drug Interactions Between Cipro and Flagyl
Ciprofloxacin (Cipro) and metronidazole (Flagyl) can interact, primarily affecting how your body processes each drug. This interaction isn’t always significant, but it warrants awareness.
Reduced Ciprofloxacin Effectiveness: Metronidazole can potentially decrease the effectiveness of ciprofloxacin. This happens because metronidazole can inhibit the liver’s enzymes that metabolize ciprofloxacin, resulting in lower ciprofloxacin levels in your blood. This might mean your Cipro treatment is less effective against the targeted infection.
Increased Risk of Side Effects: While uncommon, the combined use might increase the likelihood of experiencing side effects associated with either medication. These can include nausea, vomiting, diarrhea, and dizziness. Monitor yourself closely for any unusual symptoms.
Dosage Adjustments: Your doctor might adjust your dosage of either medication or recommend alternative antibiotics to minimize potential interactions. Always inform your doctor about all medications you are taking, including over-the-counter drugs and supplements.
Specific Concerns: If you have liver or kidney problems, this interaction requires extra caution. Discuss this with your healthcare provider before starting treatment with both medications.
Monitoring: Regular monitoring by your healthcare provider is recommended, especially during the course of combined treatment. They can assess the effectiveness of the therapy and adjust it if necessary.
Alternative Treatment: In some cases, your doctor may prescribe alternative antibiotics that don’t interact as significantly. This is a possibility if the interaction risk is deemed high or you exhibit negative reactions.
Considerations for Concurrent Use or Sequential Treatment
Ciprofloxacin (Cipro) and metronidazole (Flagyl) are often used to treat infections, sometimes concurrently or sequentially. However, combining or following these antibiotics requires careful consideration due to potential drug interactions and individual patient factors.
Concurrent Use: Potential Interactions
- Antagonistic Effects: While not always significant, some studies suggest potential antagonistic effects when Cipro and Flagyl are used concurrently against certain bacteria. Consult clinical guidelines for specific pathogens.
- Increased Risk of Side Effects: Combining these medications may increase the likelihood of experiencing gastrointestinal upset, nausea, or diarrhea. Careful monitoring is warranted.
- Pharmacokinetic Interactions: Although generally considered minor, minor alterations in metabolism can occur. Your doctor will consider your individual metabolism and adjust dosages if necessary.
Sequential Treatment: Strategies and Timing
- Infection Severity and Type: The choice between concurrent or sequential use heavily depends on the severity and type of infection. For instance, severe infections might benefit from concurrent therapy.
- Individual Patient Factors: Age, underlying health conditions, and concurrent medications all influence the decision-making process. Your physician should always be consulted.
- Duration of Treatment: The duration of each antibiotic course depends on the specific infection, bacterial sensitivity, and the patient’s response. Standard treatment regimens should be followed unless specifically advised otherwise by a physician.
- Monitoring: Regular clinical evaluation and monitoring for adverse reactions are imperative during both concurrent and sequential treatment.
Specific Recommendations
Always discuss the optimal treatment strategy with your physician. They will weigh the benefits and risks based on your specific situation. They should provide detailed information about potential side effects and how to manage them effectively.
Alternative Treatments
Remember, other antibiotic combinations or alternative therapies may be more suitable depending on the infection’s nature and the patient’s health status. Explore all treatment options with your doctor to find the best course of action.