Ciprofloxacin (Cipro) is not typically the first-line treatment for staph skin infections. Staphylococcus aureus, the bacteria responsible for many skin infections, often exhibits resistance to fluoroquinolones like Cipro. Therefore, your doctor will likely prescribe other antibiotics with higher efficacy against common staph strains.
However, in specific situations, Cipro might be considered. This depends heavily on the severity of the infection, the specific type of staph bacteria identified (through culture and sensitivity testing), and your medical history, including any prior antibiotic use and allergies. This is because some less common staph strains might be susceptible to Cipro.
Always consult your physician before using Cipro or any antibiotic for a staph skin infection. Self-treating can lead to complications, including the development of antibiotic-resistant bacteria, which makes future treatment far more challenging. Proper diagnosis and tailored treatment are paramount for successful recovery.
Your doctor will assess your condition, order necessary tests, and prescribe the most appropriate medication and treatment plan. This may involve other antibiotics, such as clindamycin or Bactrim, or potentially topical treatments depending on the infection’s nature and extent. Following your doctor’s instructions meticulously is critical for optimal results and avoiding potential side effects.
- Cipro for Staph Skin Infection: A Detailed Overview
- What is a Staph Skin Infection?
- Types of Staph Skin Infections
- Symptoms to Watch For
- Is Ciprofloxacin Effective Against Staph?
- Understanding Ciprofloxacin’s Mechanism of Action
- Appropriate Dosage and Administration of Ciprofloxacin
- Potential Side Effects and Risks of Ciprofloxacin
- When to Seek Alternative Treatments for Staph Infections
- Severe or Complicated Infections
- Allergic Reactions
- Underlying Health Conditions
- Recurring Infections
- Preventing Staph Skin Infections
Cipro for Staph Skin Infection: A Detailed Overview
Ciprofloxacin (Cipro) is not typically the first-line treatment for staph skin infections. Staphylococcus aureus, the common cause of these infections, often exhibits resistance to Cipro.
However, Cipro might be considered in specific situations, such as a serious infection where other antibiotics have failed or when the infecting strain is known to be susceptible to Cipro.
Always obtain a bacterial culture and sensitivity test before starting any antibiotic. This test identifies the specific bacteria causing the infection and determines its susceptibility to various antibiotics, ensuring optimal treatment.
Treatment decisions should be made by your physician based on your individual circumstances and test results. Self-treating with Cipro or any antibiotic can worsen the infection and lead to antibiotic resistance.
| Factor | Relevance to Cipro Use |
|---|---|
| Infection Severity | Cipro might be considered for severe infections unresponsive to other treatments. |
| Antibiotic Resistance | Cipro resistance is common in S. aureus. Sensitivity testing is critical. |
| Patient Allergies | Alternatives must be considered if the patient is allergic to Cipro or fluoroquinolones. |
| Specific Strain | If the infecting strain is known to be Cipro-susceptible, it might be an option. |
Possible side effects of Cipro include nausea, diarrhea, and headache. More serious side effects are rare but possible and include tendonitis and nerve damage. Report any adverse reactions to your doctor immediately.
Remember: This information is for educational purposes only and should not be considered medical advice. Always consult a healthcare professional for diagnosis and treatment of staph skin infections.
What is a Staph Skin Infection?
Staph skin infections are caused by Staphylococcus bacteria, commonly found on skin and in noses. These infections range from minor irritations to serious, potentially life-threatening conditions. Several types of staph bacteria can cause infection; Staphylococcus aureus (often called “staph”) is the most common and can cause a wide variety of skin problems.
Types of Staph Skin Infections
- Boils (furuncles): Painful, pus-filled bumps usually developing from a hair follicle.
- Carbuncles: Clusters of boils joined together under the skin.
- Impetigo: Highly contagious infection causing blisters and sores, commonly in children.
- Cellulitis: Deeper skin infection characterized by swelling, redness, and pain.
- Folliculitis: Infection of hair follicles, often manifesting as small, inflamed bumps.
Symptoms to Watch For
Symptoms vary depending on the type of infection but often include: redness, swelling, pain, pus or drainage, warmth to the touch, fever. Seek medical attention if you experience spreading redness, severe pain, or high fever.
- Note: This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for diagnosis and treatment.
Proper hygiene, including regular handwashing and avoiding contact with infected areas, helps prevent the spread of staph infections.
Is Ciprofloxacin Effective Against Staph?
Ciprofloxacin’s effectiveness against staph infections varies significantly depending on the specific type of staphylococcus bacteria.
Ciprofloxacin, a fluoroquinolone antibiotic, generally works well against some strains of Staphylococcus aureus, but not against many methicillin-resistant Staphylococcus aureus (MRSA) infections. MRSA is a major concern because it’s resistant to many common antibiotics.
- Ciprofloxacin is typically not the first-line treatment for staph skin infections. Doctors usually prefer antibiotics like dicloxacillin, clindamycin, or bactrim for susceptible strains.
- MRSA infections require different antibiotics. Treatment options for MRSA include vancomycin, linezolid, daptomycin, or ceftaroline. Your doctor will determine the best antibiotic based on lab results identifying the specific strain of staph.
- Always consult a healthcare provider for diagnosis and treatment. Self-treating a staph infection can be dangerous and may lead to antibiotic resistance. A proper diagnosis ensures you receive the correct medication.
Laboratory testing is crucial to determine antibiotic susceptibility. Your doctor will send a sample for culture and sensitivity testing, which helps identify the specific bacteria and determine the most effective antibiotic. This ensures the most appropriate treatment and helps avoid ineffective therapies.
- Obtain a proper diagnosis. A clinical examination and lab tests are necessary.
- Follow your doctor’s instructions carefully. Complete the prescribed course of antibiotics, even if you feel better before finishing.
- Practice good hygiene. Washing your hands frequently and keeping wounds clean can help prevent infections.
Remember, this information is for educational purposes and does not constitute medical advice. Always seek professional medical guidance for any health concerns.
Understanding Ciprofloxacin’s Mechanism of Action
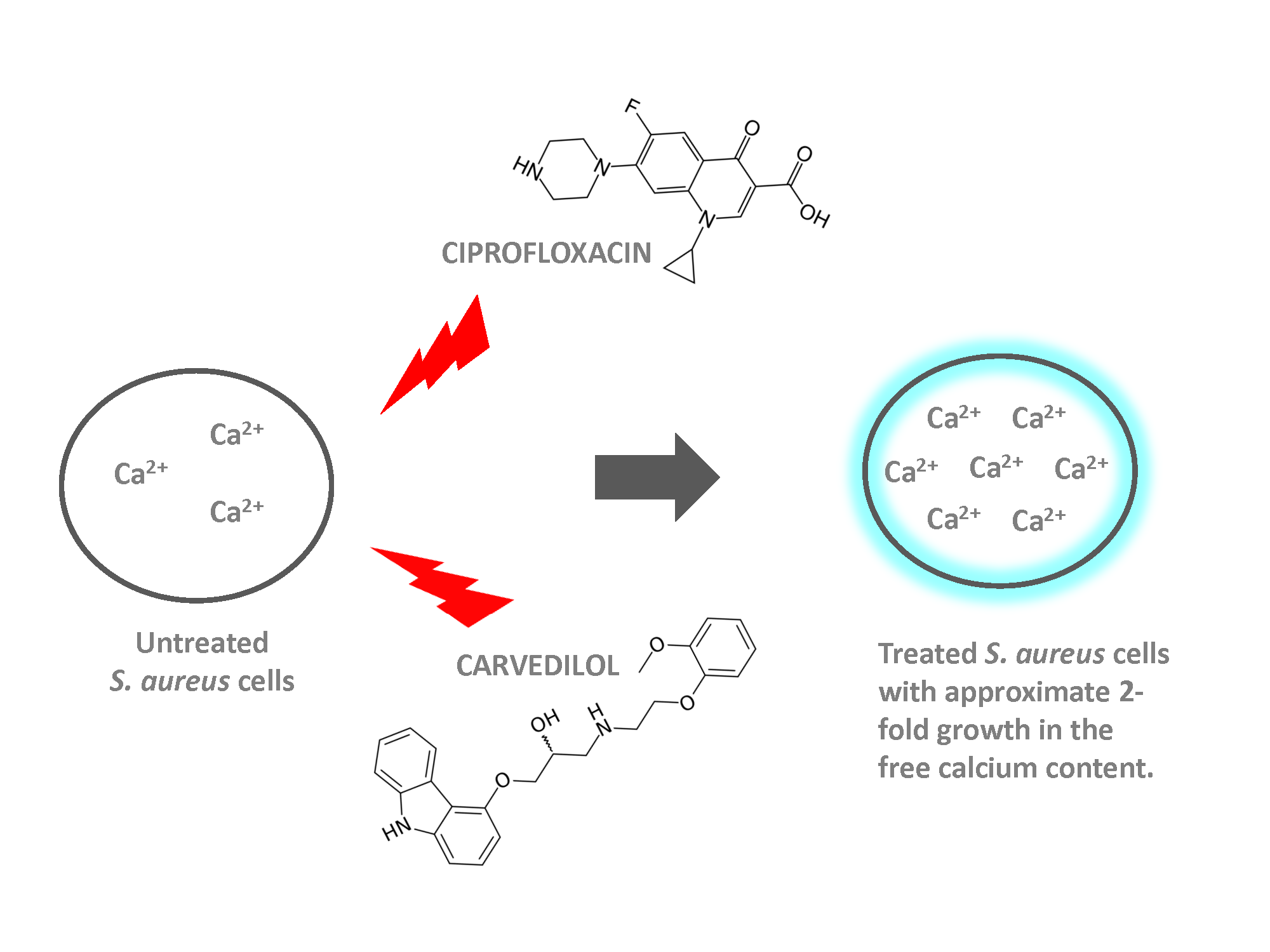
Ciprofloxacin, a fluoroquinolone antibiotic, targets bacterial DNA gyrase and topoisomerase IV. These enzymes are crucial for DNA replication, transcription, and repair in bacteria.
By inhibiting these enzymes, ciprofloxacin prevents bacteria from properly unwinding and replicating their DNA. This halts bacterial growth and ultimately leads to bacterial cell death.
The precise mechanism involves binding to these enzymes, creating a complex that prevents DNA strand separation. This blockage disrupts the normal cellular processes, causing bacterial cell death.
Ciprofloxacin’s effectiveness against Staphylococcus aureus (Staph) depends on the bacteria’s susceptibility. Some strains possess resistance mechanisms, rendering ciprofloxacin ineffective. Therefore, susceptibility testing is critical before treatment.
Remember, ciprofloxacin is not always the first-line treatment for staph skin infections. Your doctor will consider several factors before prescribing it, including the severity of the infection and the patient’s medical history.
Appropriate Dosage and Administration of Ciprofloxacin
Ciprofloxacin dosage for staph skin infections varies depending on the severity of the infection and the patient’s individual factors. Always follow your doctor’s prescribed dosage and duration. Typical oral dosages range from 250mg to 750mg twice daily. The medication should be taken with a full glass of water, ideally at least two hours before or after taking antacids or multivitamins containing minerals like iron or zinc to maximize absorption.
Intravenous administration may be necessary for severe infections. Dosage and infusion rate are determined by the prescribing physician. Always complete the full course of antibiotics, even if symptoms improve. Stopping early can lead to recurrence or development of antibiotic-resistant bacteria.
Common side effects include nausea, diarrhea, and abdominal pain. More serious side effects, though rare, include tendonitis or tendon rupture. Seek immediate medical attention if you experience severe pain or swelling in a joint. Discuss any concerns or questions about potential side effects with your physician or pharmacist before starting treatment.
Remember, this information is for general knowledge and does not replace professional medical advice. Always consult with your doctor or other qualified healthcare provider before starting or altering any medication regimen. They will carefully assess your condition and determine the most appropriate treatment plan for you.
Potential Side Effects and Risks of Ciprofloxacin
Ciprofloxacin, while effective against some bacteria, carries potential side effects. Common reactions include nausea, diarrhea, and abdominal pain. These typically resolve without intervention. However, more serious reactions demand immediate medical attention.
Gastrointestinal Issues: Severe diarrhea, possibly indicating Clostridium difficile infection (a serious complication), needs prompt medical evaluation. Dehydration can result from prolonged diarrhea or vomiting. Report these symptoms to your doctor.
Nervous System Effects: Dizziness, headache, and lightheadedness are possible. Rare but serious neurological side effects include seizures, confusion, and hallucinations. Seek medical assistance if you experience any unusual neurological symptoms.
Allergic Reactions: Although uncommon, allergic reactions, ranging from skin rash to life-threatening anaphylaxis, can occur. Stop taking Ciprofloxacin and seek immediate medical care if you develop a rash, hives, swelling, or difficulty breathing.
Tendinitis and Tendon Rupture: This is a noteworthy risk, particularly in older adults or those taking corticosteroids concurrently. Pain or inflammation in tendons, especially in the Achilles tendon, warrants immediate medical assessment and possibly cessation of Ciprofloxacin.
Note: This information is not exhaustive. Always consult your doctor or pharmacist for complete information on potential side effects and interactions, and report any concerning symptoms immediately. They can help assess your specific risk factors and provide personalized advice.
When to Seek Alternative Treatments for Staph Infections
If Ciprofloxacin (Cipro) fails to improve your staph infection within 48-72 hours, or if symptoms worsen, consult your doctor immediately. This suggests the infection may be resistant to Cipro, requiring a different antibiotic.
Severe or Complicated Infections
Seek alternative treatment options if your staph infection shows signs of severity, such as spreading rapidly, involving deep tissues, causing high fever (over 101°F), or leading to noticeable pus or abscess formation. These indicators necessitate a stronger antibiotic or surgical intervention.
Allergic Reactions
Stop taking Cipro and contact your doctor immediately if you experience any allergic reaction, including skin rash, itching, swelling, difficulty breathing, or dizziness. Your doctor will prescribe a different antibiotic that is safe for you.
Underlying Health Conditions
Individuals with weakened immune systems (e.g., due to HIV, cancer treatment, or diabetes) should discuss treatment options with their doctor promptly. They may require stronger antibiotics or additional supportive care to manage their infection effectively.
Recurring Infections
Recurrent staph infections necessitate a thorough evaluation to identify underlying causes and develop a tailored treatment plan. This might involve specialist consultation and long-term antibiotic regimens or alternative therapies like bacteriophage therapy.
Preventing Staph Skin Infections
Wash your hands frequently with soap and water for at least 20 seconds, especially after touching potentially contaminated surfaces or people. Thoroughly clean any cuts or scrapes with soap and water, and apply a clean bandage.
Avoid sharing personal items like towels, razors, and clothing. These items can easily harbor staph bacteria.
Keep cuts and scrapes covered until they are completely healed to prevent bacteria from entering your body. Change bandages regularly and wash your hands each time you do so.
Practice good hygiene. Shower or bathe regularly, keeping your skin clean and dry, especially in areas prone to sweating.
If you have a staph infection, follow your doctor’s treatment plan meticulously to prevent spreading the infection to others or yourself. Avoid touching the infected area unless necessary for cleaning and treatment, and always wash your hands afterwards.
Boost your immune system by maintaining a healthy diet, getting enough sleep, and managing stress. A stronger immune system helps your body fight off infections more effectively.
If you participate in contact sports, keep your skin clean and use antiseptic wipes to help prevent spreading bacteria. Immediately treat any open wounds.
Monitor your skin regularly for any signs of infection such as redness, swelling, pus, or pain. Seek medical attention promptly if you suspect a staph infection.