Doxycycline isn’t your first-line defense against anaerobic infections. Instead, consider clindamycin or metronidazole as primary treatment options. These antibiotics demonstrate superior efficacy against a broader spectrum of anaerobic bacteria commonly causing infections.
However, doxycycline can play a supporting role. Its effectiveness against certain anaerobic species, like Bacteroides fragilis (though limited), makes it a viable addition in specific cases, particularly polymicrobial infections involving both aerobic and anaerobic pathogens. Always conduct susceptibility testing to guide treatment decisions.
Remember, the clinical context is paramount. Factors like infection site, patient history (allergies, previous treatment failures), and the suspected causative organisms significantly influence antibiotic selection. Consult current guidelines and local antibiograms for the most up-to-date recommendations. This allows for precise, targeted therapy.
Specific anaerobic infections where doxycycline might be considered as an adjunct: Some pelvic inflammatory diseases (PID) involving mixed flora, or certain skin and soft tissue infections (SSTIs) might benefit from this approach, in conjunction with a primary anaerobic antibiotic. Always discuss this strategy with a qualified medical professional.
Caution: Doxycycline’s activity against anaerobes is significantly weaker than against aerobes. Over-reliance on doxycycline for anaerobic infections increases the risk of treatment failure and potential complications.
- Doxycycline and Anaerobic Bacteria: A Detailed Overview
- Doxycycline’s Mechanism of Action Against Bacteria
- Anaerobic Bacteria Susceptibility to Doxycycline
- Gram-Positive Anaerobes
- Gram-Negative Anaerobes
- Factors Affecting Susceptibility
- Clinical Indications for Doxycycline in Anaerobic Infections
- Limitations of Doxycycline Against Anaerobic Bacteria
- Common Anaerobic Infections Treated with Doxycycline
- Skin and Soft Tissue Infections
- Pelvic Inflammatory Disease (PID)
- Other Infections
- Important Considerations
- Limitations of Doxycycline in Anaerobic Infections
- Doxycycline Dosage and Administration for Anaerobic Infections
- Specific Considerations
- Patient-Specific Factors
- Potential Side Effects and Drug Interactions
- Gastrointestinal Issues
- Other Potential Side Effects
- Drug Interactions
- Significant Interactions
- Alternatives to Doxycycline for Anaerobic Infections
- Alternative Antibiotics based on Infection Site
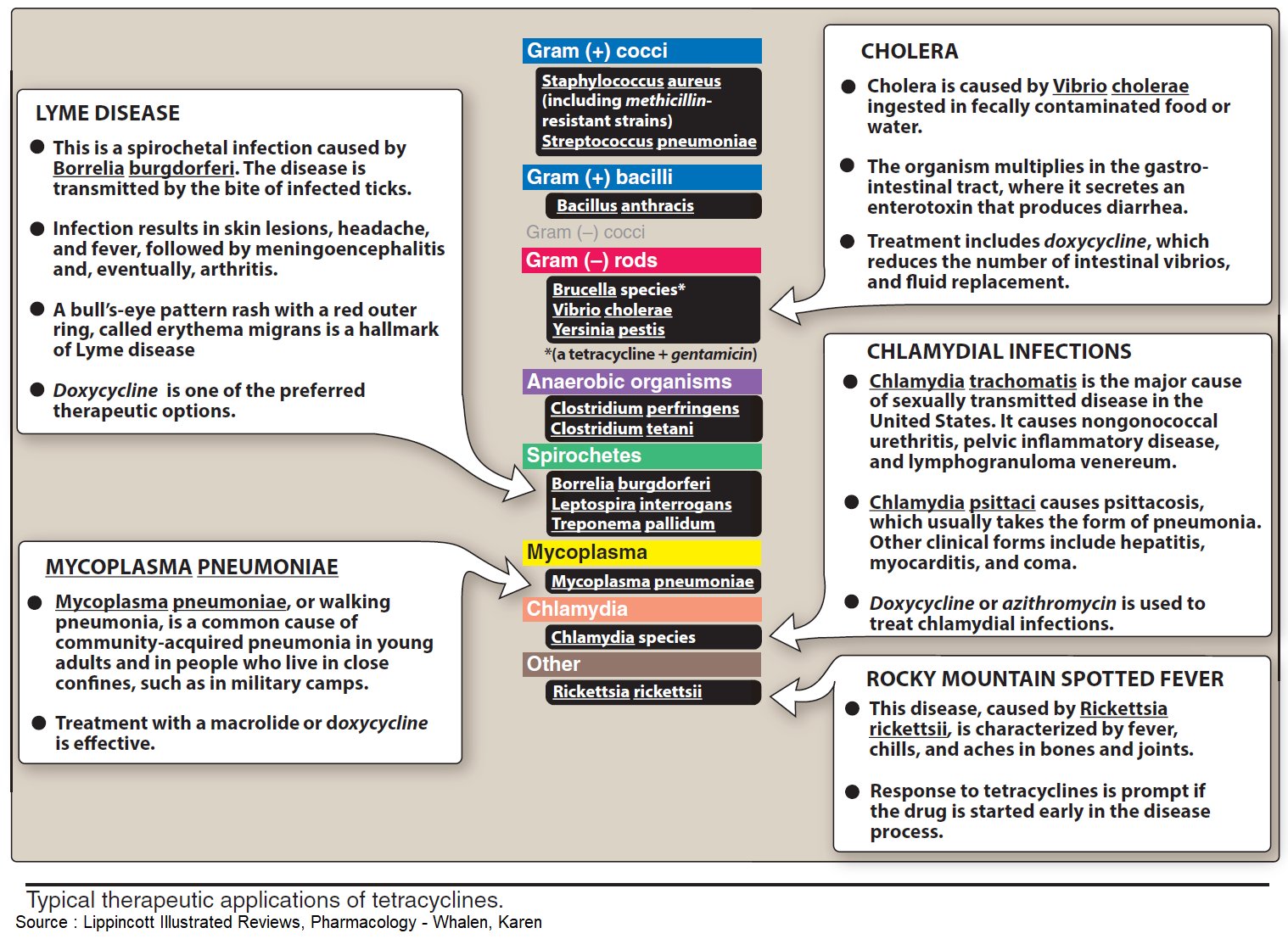
Doxycycline and Anaerobic Bacteria: A Detailed Overview
Doxycycline’s effectiveness against anaerobic bacteria is limited. While it exhibits some activity against certain species, it’s not a first-line treatment.
Bacteroides fragilis, a common anaerobic bacterium found in the gut, shows variable susceptibility. Some strains demonstrate resistance, highlighting the need for susceptibility testing before treatment.
Doxycycline’s mechanism of action, targeting bacterial protein synthesis, is less effective against anaerobes compared to other antibiotics like metronidazole or clindamycin. These latter drugs directly disrupt anaerobic metabolism.
Clinical situations where doxycycline might be considered in combination therapy with other antibiotics against anaerobic infections include mixed infections involving both aerobic and anaerobic bacteria. However, careful selection based on susceptibility testing is paramount.
For severe anaerobic infections, metronidazole or clindamycin are generally preferred due to their superior activity and broader spectrum against a wider range of anaerobic bacteria.
Always consult current antimicrobial guidelines and local antibiograms for the most up-to-date recommendations on treating anaerobic infections. Consider factors like infection site and patient history when choosing a treatment regimen.
Research continues to refine our understanding of doxycycline’s interaction with anaerobic bacteria. Monitoring treatment response and adapting therapy based on clinical findings is crucial for optimal patient outcomes.
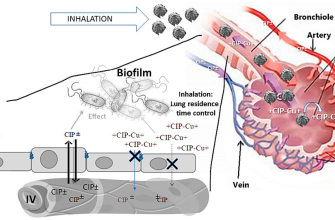
Doxycycline’s Mechanism of Action Against Bacteria
Doxycycline inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit. This interaction prevents the attachment of aminoacyl-tRNA to the acceptor site on the mRNA-ribosome complex. Consequently, the bacteria cannot elongate polypeptide chains, halting protein production.
Specifically, doxycycline binds reversibly to the 30S ribosomal subunit at the A site, interfering with the binding of aminoacyl-tRNA molecules. This blockage prevents the addition of new amino acids to the growing peptide chain. The result is a disruption of bacterial protein synthesis, leading to bacterial cell death.
This mechanism is particularly effective against a broad range of bacteria, including many that are susceptible to tetracycline antibiotics. The drug’s effectiveness stems from its ability to penetrate bacterial cell walls and reach the ribosomes. This access is key to its action and contributes to its efficacy.
Note: While doxycycline is broadly effective, resistance mechanisms exist. These mechanisms often involve alterations in the bacterial ribosome or active efflux pumps that remove the drug from the bacterial cell. These should be considered when selecting antibiotic therapy.
In summary: Doxycycline’s primary mechanism involves direct inhibition of bacterial protein synthesis at the ribosomal level. This is achieved through binding to the 30S ribosomal subunit, preventing peptide chain elongation and ultimately leading to bacterial cell death.
Anaerobic Bacteria Susceptibility to Doxycycline
Doxycycline’s activity against anaerobic bacteria is limited, varying significantly depending on the specific species. While it demonstrates some effectiveness against certain anaerobic bacteria, it’s generally not the first-line treatment choice.
Gram-Positive Anaerobes
- Actinomyces species: Doxycycline exhibits moderate activity. Consider combining with other antibiotics for optimal results.
- Clostridium species: Susceptibility is highly variable. Some strains show resistance. Use alternative antibiotics like metronidazole or clindamycin.
- Propionibacterium acnes: Doxycycline is frequently used, often successfully in treating acne vulgaris, a condition often complicated by the presence of this anaerobic bacteria.
Gram-Negative Anaerobes
- Bacteroides fragilis: Generally resistant to doxycycline. Metronidazole is the preferred treatment.
- Prevotella species: Show variable susceptibility; often require combination therapy.
- Fusobacterium species: Susceptibility varies, making alternative antibiotics a safer choice.
Always consider factors like the specific bacterial species, the site of infection, and the patient’s overall health when choosing an antibiotic regimen. Antibiotic susceptibility testing is recommended whenever possible to guide treatment decisions.
Factors Affecting Susceptibility
- Bacterial Strain: Genetic variations within a species affect antibiotic response.
- Dosage and Duration: Inadequate dosing or treatment duration can lead to treatment failure.
- Combination Therapy: Combining doxycycline with another antibiotic (such as metronidazole) often enhances effectiveness against anaerobic infections.
Consult current guidelines and expert recommendations for the most up-to-date information on antibiotic choices for anaerobic infections.
Clinical Indications for Doxycycline in Anaerobic Infections
Doxycycline’s use against anaerobic bacteria is often adjunctive, meaning it’s used alongside other antibiotics. It’s particularly valuable in treating infections caused by Bacteroides fragilis, a common anaerobic bacterium found in the gut. Consider doxycycline for polymicrobial infections involving both aerobic and anaerobic pathogens, especially in cases of intra-abdominal infections or pelvic inflammatory disease (PID).
Doxycycline exhibits activity against several anaerobic species, including Prevotella and Porphyromonas species, frequently encountered in oral and periodontal infections. For severe or complicated infections, combine doxycycline with metronidazole or clindamycin for broader coverage. Remember that susceptibility testing guides optimal antibiotic selection.
While doxycycline demonstrates some effectiveness against anaerobic bacteria, it’s not the first-line choice for most anaerobic infections. Its role is mainly supplementary, improving treatment outcomes in polymicrobial scenarios where anaerobic species contribute significantly to the infection. Always consult current guidelines and laboratory data to guide treatment decisions.
Specific examples include its use in treating acute bacterial exacerbations of chronic obstructive pulmonary disease (AECOPD) when anaerobic bacteria are suspected and in cases of aspiration pneumonia, where a mixed infection is likely. Doxycycline’s broad spectrum, coupled with its good tissue penetration, makes it a valuable tool in these situations.
Dosage and duration of treatment depend entirely on the specific infection, patient factors, and local antibiotic resistance patterns. Close monitoring of the patient’s response to therapy is paramount. Always adhere to prescribed dosages and treatment duration.
Limitations of Doxycycline Against Anaerobic Bacteria
Doxycycline’s effectiveness against anaerobic bacteria is limited. It primarily targets bacteria requiring oxygen for growth (aerobic bacteria) and displays significantly reduced activity against many anaerobic species.
Many anaerobic bacteria possess inherent resistance mechanisms, including reduced drug permeability and efflux pumps that actively remove doxycycline from the cell. This intrinsic resistance renders many treatments with doxycycline ineffective.
Specific anaerobic bacteria like Bacteroides fragilis, a common gut inhabitant, demonstrate high levels of resistance. Therefore, doxycycline is rarely a first-line treatment for infections caused by these organisms.
Clinicians should consider susceptibility testing when treating anaerobic infections. This testing helps determine the optimal antibiotic based on the specific pathogen involved, ensuring the most appropriate treatment strategy.
Alternative antibiotics, such as metronidazole or clindamycin, are usually preferred for anaerobic infections. These agents effectively inhibit anaerobic bacterial growth and often represent superior therapeutic options.
For mixed infections, containing both aerobic and anaerobic bacteria, a combination therapy incorporating both doxycycline and an anaerobic-specific antibiotic is sometimes warranted. This approach is best determined on a case-by-case basis, considering individual patient factors and the results of susceptibility testing.
Common Anaerobic Infections Treated with Doxycycline
Doxycycline’s broad-spectrum activity makes it useful against certain anaerobic bacteria, although it’s not a first-line treatment for most anaerobic infections. Its effectiveness varies depending on the specific anaerobic species involved.
Skin and Soft Tissue Infections
Doxycycline can be part of a treatment regimen for some skin and soft tissue infections caused by anaerobic bacteria, particularly when combined with other antibiotics like metronidazole. This is often the case in severe cases or mixed infections.
Pelvic Inflammatory Disease (PID)
In cases of PID where anaerobic bacteria are suspected, doxycycline may be included in the antibiotic combination to improve coverage. However, treatment protocols frequently prioritize other antibiotics with better anaerobic activity.
Other Infections
While less common, doxycycline might be considered in treating certain atypical pneumonias or intra-abdominal infections when anaerobic bacteria are a suspected component. However, other antibiotics typically provide superior anaerobic coverage in these scenarios.
Important Considerations
| Infection Type | Doxycycline Role | Usual Combination Therapy |
|---|---|---|
| Skin & Soft Tissue | Adjunctive therapy | Metronidazole, clindamycin |
| Pelvic Inflammatory Disease | Part of broad-spectrum regimen | Cefoxitin, metronidazole |
| Atypical Pneumonia | Possible adjunctive agent | Macrolides, β-lactams |
Limitations of Doxycycline in Anaerobic Infections
Remember, doxycycline’s activity against anaerobes is limited compared to drugs specifically designed for these bacteria. Always consult current guidelines and consider susceptibility testing before prescribing.
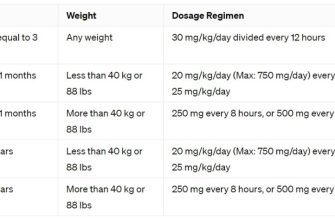
Doxycycline Dosage and Administration for Anaerobic Infections
Doxycycline’s effectiveness against anaerobic bacteria depends heavily on the specific infection and the infecting organism. Generally, for treating anaerobic infections, a dosage of 100-200 mg twice daily is recommended. This regimen is usually continued for at least 7-10 days, potentially longer depending on clinical response.
Specific Considerations
Treatment Duration: Observe the patient closely. Extend treatment if symptoms persist or recur. A shorter course may suffice for less severe infections, but a longer course is often necessary for deep-seated or severe infections, such as pelvic inflammatory disease or intra-abdominal infections.
Combination Therapy: Doxycycline is frequently combined with other antibiotics, like metronidazole or clindamycin, to broaden its antimicrobial spectrum and achieve synergy against a wider range of anaerobic bacteria. This combination often improves treatment outcomes, especially in mixed infections.
Patient-Specific Factors
Dosage adjustments may be necessary for patients with impaired renal or hepatic function. Consult relevant guidelines for appropriate dosage modifications in these cases. Always consider factors like age, weight, and overall health status when determining the optimal dosage and duration of treatment. Regular monitoring of the patient’s response is also critical.
Important Note: This information is for guidance only and should not replace consultation with a medical professional. Always refer to current medical guidelines and consult with a physician before initiating or altering any antibiotic treatment regimen.
Potential Side Effects and Drug Interactions
Doxycycline, while effective against certain anaerobic bacteria, can cause several side effects. These vary in severity and frequency.
Gastrointestinal Issues
- Nausea and vomiting are common, often resolving with continued use or after dosage adjustments. Consider taking doxycycline with food to mitigate this.
- Diarrhea can occur; severe diarrhea may indicate Clostridium difficile infection, requiring immediate medical attention.
- Esophageal irritation can happen, especially if taking the medication without sufficient water. Always swallow doxycycline with a full glass of water.
Other Potential Side Effects
- Photosensitivity: increased sun sensitivity leading to sunburn. Use sunscreen and protective clothing while taking doxycycline.
- Yeast infections: particularly in women. Consult your doctor if you experience vaginal itching or discharge.
- Headache and dizziness are possible. Inform your physician if these persist or worsen.
Drug Interactions
Doxycycline interacts with several medications. It’s crucial to inform your doctor of all medications, supplements, and herbal remedies you’re taking. Here are some key examples:
Significant Interactions
- Antacids: Reduce doxycycline absorption. Separate administration by several hours.
- Warfarin: May increase the risk of bleeding. Close monitoring of blood clotting is needed.
- Calcium supplements: May reduce doxycycline absorption. Maintain a separation in dosage timing.
- Birth control pills: Reduced effectiveness of oral contraceptives. Consider alternative birth control methods.
This information is not exhaustive. Always consult your physician or pharmacist before starting or stopping any medication, including doxycycline, and report any adverse effects immediately.
Alternatives to Doxycycline for Anaerobic Infections
Clinicians often select metronidazole as a primary alternative. It demonstrates strong activity against a wide range of anaerobic bacteria, including Bacteroides fragilis and Clostridium difficile. Consider dosage adjustments based on the specific infection and patient factors. For severe infections or those unresponsive to metronidazole, consider carbapenems like imipenem or meropenem. These broad-spectrum antibiotics offer reliable coverage against many anaerobic species.
Alternative Antibiotics based on Infection Site
The optimal antibiotic choice depends heavily on the infection location. For intra-abdominal infections, consider piperacillin-tazobactam, which exhibits good activity against both aerobic and anaerobic pathogens. In pelvic infections, clindamycin is frequently used, although resistance patterns should be monitored. For brain abscesses, a combination therapy, potentially including ceftriaxone and metronidazole, might be necessary due to the potential involvement of both aerobic and anaerobic organisms.
Always consult current antimicrobial susceptibility data for your region to guide antibiotic selection. Clinical response monitoring is crucial for ensuring successful treatment. If treatment fails, reevaluation and potential change in antibiotic therapy are recommended. Remember, these suggestions provide general guidance and should not substitute for professional medical advice tailored to each individual case.