Doxycycline and clindamycin are sometimes used to treat methicillin-resistant Staphylococcus aureus (MRSA) infections, but their effectiveness varies significantly depending on the specific strain and infection site. Clinicians should prioritize susceptibility testing before prescribing either antibiotic.
Staphylococcus aureus strains exhibiting resistance to erythromycin frequently also display resistance to clindamycin. Therefore, a D-test is crucial before prescribing clindamycin to determine its efficacy. A positive D-test indicates clindamycin resistance. This simple test dramatically impacts treatment choices.
Doxycycline generally demonstrates broader activity against MRSA than clindamycin. However, both antibiotics possess limitations. Their use should be guided by local antibiotic resistance patterns and considered only when other, more potent options are unsuitable or unavailable. Always confirm susceptibility before treatment initiation to avoid treatment failures and promote responsible antibiotic stewardship.
Remember: These recommendations are for informational purposes only and should not replace guidance from a qualified healthcare professional. Treatment decisions must be made on a case-by-case basis, considering individual patient factors and infection characteristics.
- Doxycycline and Clindamycin for MRSA: A Detailed Overview
- Understanding MRSA and its Treatment Challenges
- Doxycycline’s Role in MRSA Infection Management
- Clindamycin’s Effectiveness Against MRSA: Considerations and Limitations
- Factors Affecting Clindamycin’s Efficacy
- Alternative Treatment Strategies
- Recommended Actions
- Limitations of Clindamycin Use Against MRSA
- Comparing Doxycycline and Clindamycin: Which is Better?
- Practical Implications and Future Directions in MRSA Treatment
Doxycycline and Clindamycin for MRSA: A Detailed Overview
Doxycycline and clindamycin are sometimes considered for treating methicillin-resistant Staphylococcus aureus (MRSA) infections, but their use requires careful consideration due to variable susceptibility.
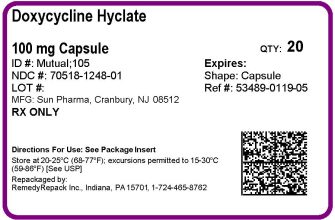
Doxycycline: This tetracycline antibiotic exhibits varying efficacy against MRSA. Susceptibility testing is crucial before prescribing. Resistance is common, so relying solely on doxycycline without lab confirmation is risky. It’s often reserved for mild infections when other options aren’t suitable or are contraindicated. Potential side effects include nausea, vomiting, and photosensitivity.
- Use: Primarily for skin and soft tissue infections, sometimes considered for pneumonia, though data is limited.
- Limitations: High rates of resistance; not suitable for serious MRSA infections.
Clindamycin: A lincosamide antibiotic, clindamycin may be effective against some MRSA strains. However, similar to doxycycline, in vitro susceptibility testing is mandatory. Clindamycin resistance is also a significant concern. C. difficile-associated diarrhea is a potential, serious adverse effect.
- Use: Skin and soft tissue infections are primary candidates, but only after susceptibility testing confirms its effectiveness.
- Limitations: High potential for resistance; C. difficile risk; not suitable for serious systemic infections.
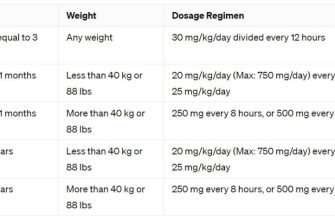
Treatment Guidelines: The Infectious Diseases Society of America (IDSA) and other leading organizations strongly advocate for susceptibility testing before initiating treatment with doxycycline or clindamycin for suspected MRSA infections. They generally recommend other agents like vancomycin, linezolid, or daptomycin for serious infections due to their higher efficacy and better safety profiles against MRSA.
- Always conduct susceptibility testing. This is non-negotiable for appropriate antibiotic stewardship.
- Reserve doxycycline and clindamycin for mild to moderate, localized skin infections. These should only be used when resistance testing shows susceptibility and alternative options are not feasible.
- Closely monitor patients for adverse reactions and treatment failure.
- Consult with an infectious disease specialist for complex cases or severe infections.
This information is for educational purposes and does not constitute medical advice. Always consult with a healthcare professional for diagnosis and treatment of MRSA infections.
Understanding MRSA and its Treatment Challenges
MRSA, or methicillin-resistant Staphylococcus aureus, is a bacterium resistant to many common antibiotics. This resistance makes MRSA infections difficult to treat, often requiring longer treatment courses and stronger medications. The severity varies; some cause minor skin infections, while others lead to life-threatening conditions like pneumonia or bloodstream infections. Accurate diagnosis through laboratory testing is key for effective management.
Treatment options depend heavily on the infection’s location and severity. Oral antibiotics, like doxycycline and clindamycin, are sometimes used for less severe skin infections, though resistance is growing. For serious infections, intravenous antibiotics, often with a combination of drugs, become necessary. This tailored approach reflects the challenge of fighting a resilient bacteria. Doctors consider factors like patient’s medical history and allergy status before deciding on a course of action.
Staphylococcus aureus itself is a common bacteria found on skin and in the nose, but its ability to develop resistance to antibiotics presents a significant public health concern. Prevention strategies, such as hand hygiene and appropriate wound care, significantly reduce transmission risk. Further complications can arise from surgical procedures where MRSA colonization can lead to post-operative infections. Therefore, preventative measures in healthcare settings are critical.
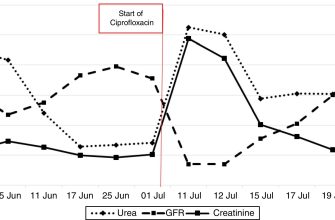
Resistance monitoring is vital. Regular testing of bacterial isolates helps track antibiotic resistance patterns and inform treatment guidelines. Developing new antibiotics and researching alternative therapies are active areas of ongoing research. The fight against MRSA requires a multi-pronged approach combining careful treatment strategies, preventative measures, and continuous scientific advancement.
Doxycycline’s Role in MRSA Infection Management
Doxycycline isn’t a first-line treatment for MRSA infections. Its use is primarily considered in situations where other antibiotics have failed or are contraindicated.
Clinical studies show doxycycline can be effective against some MRSA strains, particularly in skin and soft tissue infections. However, resistance is a growing concern, so susceptibility testing is vital before prescribing.
Doxycycline’s efficacy varies depending on the specific MRSA strain and the site of infection. It often demonstrates better activity against certain MRSA strains compared to other tetracyclines, like minocycline. However, clindamycin generally shows stronger activity in most cases.
Combination therapy using doxycycline with other agents, like rifampin, may offer advantages in specific severe infections; however, this approach requires careful monitoring due to potential drug interactions and increased risk of side effects.
The decision to use doxycycline for MRSA should involve a careful risk-benefit assessment by a healthcare professional considering factors such as the severity of the infection, patient’s medical history, and the local prevalence of resistant strains.
Always consult current guidelines and local antibiograms to inform treatment choices. Regular monitoring of therapeutic response is necessary to ensure effective treatment and timely adjustments.
Clindamycin’s Effectiveness Against MRSA: Considerations and Limitations
Clindamycin’s activity against MRSA is variable and depends heavily on the specific strain. While it can be effective in some cases, relying solely on it is risky due to high rates of resistance.
Factors Affecting Clindamycin’s Efficacy
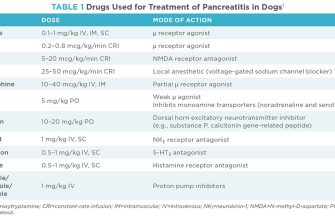
- Inducible Clindamycin Resistance (iMLSB): Many MRSA strains exhibit this resistance mechanism. They appear susceptible to clindamycin on standard susceptibility testing, but actually harbor resistance genes. This means treatment failure is likely. A D-zone test, performed alongside standard susceptibility testing, helps detect iMLSB. A positive D-test indicates the presence of iMLSB resistance, rendering clindamycin unsuitable.
- Spontaneous Resistance: Even in the absence of iMLSB, spontaneous clindamycin resistance can occur during treatment.
- Strain-Specific Susceptibility: The susceptibility of MRSA to clindamycin varies significantly between different strains and geographic locations. Local antibiograms are valuable in guiding therapy.
Alternative Treatment Strategies
Clindamycin should not be used as a monotherapy for MRSA infections. Instead, it may play a supporting role in combination therapies, particularly in severe or complicated infections where multiple drug regimens are needed. However, always prioritize proven effective alternatives.
Recommended Actions
- Perform a D-test to assess for inducible clindamycin resistance prior to treatment.
- Consult local antibiograms to determine clindamycin susceptibility rates in your region.
- Prioritize other proven antibiotics against MRSA like vancomycin, linezolid, daptomycin or ceftaroline in uncomplicated cases.
- Reserve clindamycin for combination therapy in severe MRSA infections, guided by susceptibility testing and clinical judgment, always consulting infectious disease specialist if necessary.
Limitations of Clindamycin Use Against MRSA
High resistance rates significantly limit clindamycin’s usefulness as a primary treatment for MRSA. False susceptibility readings due to iMLSB frequently lead to treatment failure. This necessitates rigorous testing and careful consideration before implementing clindamycin-based treatment plans.
Comparing Doxycycline and Clindamycin: Which is Better?
Neither doxycycline nor clindamycin is universally superior for MRSA treatment; the best choice depends on the specific infection and patient factors. Doxycycline offers broader coverage against other potential pathogens, making it suitable for infections where multiple organisms might be involved. However, clindamycin often boasts higher potency against MRSA itself.
Consider these key differences:
| Feature | Doxycycline | Clindamycin |
|---|---|---|
| MRSA Activity | Variable; often less potent than clindamycin. | Generally more potent against MRSA. |
| Spectrum of Activity | Broader; covers a wider range of bacteria. | Narrower; primarily effective against Gram-positive bacteria. |
| Adverse Effects | Common side effects include nausea, vomiting, diarrhea, and photosensitivity. | Common side effects include diarrhea, pseudomembranous colitis (a serious complication), and nausea. |
| Resistance | Increasing MRSA resistance observed. | Increasing MRSA resistance observed, but often less prevalent than doxycycline resistance. |
| Route of Administration | Oral or IV. | Oral or IV. |
Before prescribing either antibiotic, clinicians should perform a susceptibility test to determine the specific antibiotic sensitivities of the isolated MRSA strain. This test guides the optimal choice for maximum efficacy and minimizes the risk of treatment failure. Additionally, patient allergies and potential drug interactions must be carefully considered. Always consult the most up-to-date guidelines and clinical practice recommendations.
Practical Implications and Future Directions in MRSA Treatment
Doxycycline and clindamycin offer viable options for treating MRSA infections, particularly in less severe cases. However, careful consideration of antibiotic susceptibility testing is paramount. Always confirm the bacteria’s sensitivity before initiating treatment.
Monitoring treatment response is critical. Regular clinical assessments, coupled with laboratory testing when appropriate, allow for timely adjustments. Failure to respond within a reasonable timeframe mandates a change in treatment strategy, potentially involving alternative antibiotics or combination therapies.
Preventing MRSA spread is equally important. Stringent infection control measures in healthcare settings, including meticulous hand hygiene and appropriate isolation protocols, significantly reduce transmission risk. Education on good hygiene practices should extend to the community level.
Research into novel therapeutic strategies is ongoing. This includes exploring new antibiotic classes, phage therapy, and innovative approaches to immune modulation. Clinical trials are evaluating these promising avenues to combat increasingly resistant strains.
Developing new diagnostic tools, enabling rapid identification and susceptibility testing, is crucial for streamlining treatment decisions. Faster diagnosis facilitates early interventions, improving outcomes and minimizing the risk of complications. This includes point-of-care testing for more timely results.
The development of antibiotic stewardship programs is vital. These programs promote the judicious use of antibiotics, minimizing the development of further resistance. They require effective collaboration between clinicians, microbiologists, and infection control specialists.