Avoid doxycycline if you have a history of pancreatitis. Studies show a potential link between this antibiotic and acute pancreatitis, particularly in individuals with certain predisposing factors. This risk isn’t insignificant; therefore, careful consideration of alternatives is necessary.
Specifically, research suggests a correlation between doxycycline use and an increased risk of developing acute pancreatitis, especially in patients with gallstones or a history of alcohol abuse. This doesn’t mean doxycycline always causes pancreatitis, but it highlights a potential adverse effect requiring your doctor’s attention.
If your physician prescribes doxycycline, openly discuss your medical history, including any prior episodes of pancreatitis or risk factors like gallstones. Transparent communication helps your doctor make the best decision about your treatment, weighing the benefits of the antibiotic against potential risks.
Remember, this information doesn’t replace professional medical advice. Always consult your doctor before starting or stopping any medication. They can assess your individual situation and determine the most appropriate course of action.
- Doxycycline and Pancreatitis: Understanding the Link
- Doxycycline’s Mechanism of Action and Potential Side Effects
- Gastrointestinal Effects
- Other Potential Side Effects
- Drug Interactions
- Reported Cases of Pancreatitis Associated with Doxycycline Use
- Risk Factors Increasing the Likelihood of Doxycycline-Induced Pancreatitis
- Pre-existing Conditions and Drug Interactions
- Differentiating Doxycycline-Induced Pancreatitis from Other Causes
- Management and Treatment of Doxycycline-Related Pancreatitis
- Nutritional Management
- Monitoring and Assessment
- Potential Complications
- Treatment Algorithm
- Long-Term Outlook
- Prevention Strategies and Alternative Antibiotics
Doxycycline and Pancreatitis: Understanding the Link
While doxycycline isn’t a typical cause of pancreatitis, a potential association exists. Reports suggest a possible link, although research remains limited and hasn’t established a definitive causal relationship.
Here’s what we know:
- Rare Occurrence: Pancreatitis following doxycycline use is uncommon. Many people take doxycycline without experiencing this complication.
- Mechanism Unclear: The exact mechanism by which doxycycline might contribute to pancreatitis isn’t fully understood. Some theories suggest drug-induced hypersensitivity or direct toxicity to the pancreas.
- Contributing Factors: Pre-existing conditions, such as gallstones or alcohol abuse, might increase the risk of pancreatitis regardless of medication. Doxycycline might act as a trigger in susceptible individuals.
- Reporting Bias: Underreporting of adverse drug reactions can obscure the true incidence of doxycycline-induced pancreatitis.
If you experience severe abdominal pain, nausea, vomiting, or fever after starting doxycycline, seek immediate medical attention. These are potential symptoms of pancreatitis. A medical professional will conduct a thorough examination and determine the appropriate diagnosis and treatment.
Important Considerations:
- Full Medical History: Always inform your doctor about all medications you’re taking, including over-the-counter drugs and supplements, before starting any new treatment.
- Individual Risk Assessment: Your doctor will assess your individual risk factors for pancreatitis before prescribing doxycycline.
- Alternative Medications: If you have a history of pancreatitis or other relevant conditions, your doctor may consider alternative antibiotics.
This information is for educational purposes only and should not be considered medical advice. Consult your healthcare provider for personalized guidance.
Doxycycline’s Mechanism of Action and Potential Side Effects
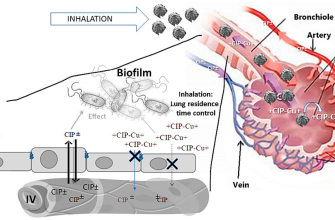
Doxycycline works by inhibiting bacterial protein synthesis. Specifically, it binds to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA to the mRNA-ribosome complex, thus halting bacterial growth and ultimately leading to bacterial cell death. This broad-spectrum antibiotic is effective against a wide range of bacteria, including those responsible for various infections.
Gastrointestinal Effects
Common side effects include nausea, vomiting, and diarrhea. These usually are mild and resolve without intervention. However, severe gastrointestinal issues are possible, though rare. Consider probiotics to mitigate these risks.
Other Potential Side Effects
Less frequent but more serious side effects can involve photosensitivity, meaning increased sensitivity to sunlight, leading to sunburns. Always use sunscreen with a high SPF when taking doxycycline. Additionally, esophageal ulcers are a risk; ensure you take the medication with plenty of water and while sitting upright. Rare cases of liver inflammation (hepatitis) and increased pressure in the brain (pseudotumor cerebri) have been reported. Immediate medical attention is needed if you experience symptoms like severe abdominal pain, jaundice (yellowing of the skin or eyes), or severe headaches.
Drug Interactions
Doxycycline can interact with several medications, including antacids, iron supplements, and some dairy products. Always inform your doctor about all medications you are taking to avoid potential interactions.
Reported Cases of Pancreatitis Associated with Doxycycline Use
While doxycycline is generally well-tolerated, reports of pancreatitis linked to its use exist. These cases are relatively rare, however, and causality isn’t always definitively established. Many reported instances involve pre-existing conditions or concurrent medications that may have contributed to the pancreatitis.
Published case studies frequently describe patients experiencing abdominal pain, nausea, and elevated pancreatic enzymes following doxycycline administration. Some studies focus on specific patient demographics or medication interactions that might increase risk. For example, older adults or those with underlying liver or gallbladder issues appear overrepresented in some reports.
The exact mechanism through which doxycycline might induce pancreatitis remains unclear. Hypotheses suggest possible direct pancreatic toxicity or indirect effects, potentially related to changes in gut microbiota or bile duct function. Further research is needed to fully elucidate this mechanism.
Clinicians should carefully consider the patient’s overall health and potential risk factors when prescribing doxycycline. A thorough medical history, including any liver or gallbladder problems, is vital. Close monitoring for signs and symptoms of pancreatitis, particularly in at-risk individuals, is recommended. If pancreatitis is suspected, doxycycline should be discontinued immediately.
Reporting suspected drug-induced pancreatitis to relevant authorities is crucial for ongoing safety monitoring and data collection. This helps to build a more complete understanding of the relationship between doxycycline and this adverse event. Transparency in reporting aids in refining prescribing practices and patient care.
Risk Factors Increasing the Likelihood of Doxycycline-Induced Pancreatitis
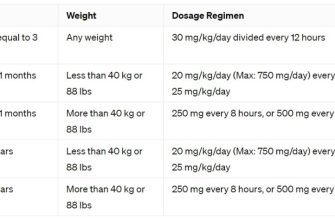
While doxycycline-induced pancreatitis is rare, certain factors significantly raise your risk. High doses of doxycycline are a primary concern. Larger than recommended dosages increase the likelihood of adverse reactions, including pancreatitis. This risk also increases with prolonged doxycycline treatment. The longer you take the medication, the greater the chance of complications. Therefore, carefully follow your doctor’s prescribed dosage and duration.
Pre-existing Conditions and Drug Interactions
Underlying health conditions also play a role. Patients with pre-existing gallbladder disease or a history of pancreatitis face a heightened risk. Concomitant medication use matters significantly. Using nonsteroidal anti-inflammatory drugs (NSAIDs) concurrently with doxycycline can increase the chance of pancreatitis. Similarly, alcohol consumption increases susceptibility to pancreatitis regardless of medication usage, so avoiding alcohol during doxycycline treatment is advisable.
Individual genetic predispositions contribute to the risk, although specific genes haven’t been definitively linked yet. This highlights the importance of informing your doctor about your family history of pancreatitis or other related conditions.
Differentiating Doxycycline-Induced Pancreatitis from Other Causes
Diagnosing doxycycline-induced pancreatitis requires careful consideration of other potential causes. Begin by obtaining a thorough patient history, including medication use, alcohol consumption, and recent illnesses. A detailed history significantly aids in differentiating drug-induced pancreatitis from other forms.
Elevated serum amylase and lipase levels suggest pancreatitis, but aren’t specific to doxycycline. Consider other medications the patient is taking. Many drugs can induce pancreatitis; excluding these possibilities is vital. A detailed review of the patient’s drug regimen is crucial.
Imaging studies, such as abdominal ultrasound or CT scan, help visualize the pancreas and assess inflammation. While these tests identify pancreatitis, they don’t pinpoint the cause. Therefore, rely on the patient’s history and drug profile for a differential diagnosis.
Gallstones are a common cause of pancreatitis. Ultrasound can help detect gallstones, allowing you to distinguish between gallstone-related and drug-induced pancreatitis. Consider this possibility especially if the patient presents with symptoms consistent with biliary tract disease.
Hypertriglyceridemia should be screened for as elevated triglyceride levels can trigger pancreatitis. A lipid panel helps determine if high triglycerides are a contributing factor.
Finally, remember that some cases remain idiopathic. If no clear cause is identified, despite thorough investigation, the possibility of idiopathic pancreatitis must be acknowledged.
Careful clinical judgment, incorporating patient history, laboratory findings, and appropriate imaging, remains the cornerstone of differentiating doxycycline-induced pancreatitis from alternative etiologies.
Management and Treatment of Doxycycline-Related Pancreatitis
Immediately discontinue doxycycline upon suspicion of pancreatitis. This is the first and most critical step.
Hospitalization is often necessary for supportive care. This includes intravenous fluids to manage dehydration and electrolyte imbalances, frequently seen in pancreatitis. Pain management is paramount; clinicians typically prescribe opioids for severe pain.
Nutritional Management
Patients usually require a temporary period of bowel rest, initially avoiding food and drink to reduce pancreatic stimulation. As symptoms subside, a gradual transition to a low-fat, easily digestible diet is implemented.
Monitoring and Assessment
Close monitoring of vital signs, amylase and lipase levels, and other relevant blood tests is crucial to track disease progression and treatment response. Regular abdominal examinations help assess pain and abdominal tenderness.
Potential Complications
Pancreatitis can lead to serious complications, including pancreatic pseudocysts, abscesses, and acute respiratory distress syndrome (ARDS). Prompt recognition and appropriate management of these complications are vital.
Treatment Algorithm
| Step | Action |
|---|---|
| 1 | Stop Doxycycline |
| 2 | Hospital Admission (Often Necessary) |
| 3 | Intravenous Fluids |
| 4 | Pain Management (Opioids) |
| 5 | Bowel Rest (Initially) |
| 6 | Gradual Diet Advancement |
| 7 | Close Monitoring (Vital signs, labs, abdominal exam) |
Long-Term Outlook
Most patients recover fully, provided they receive prompt and appropriate treatment. The long-term prognosis depends on the severity of the pancreatitis and the presence of any complications. Follow-up appointments are necessary to monitor for potential long-term issues.
Prevention Strategies and Alternative Antibiotics
Minimize your risk of pancreatitis by maintaining a healthy weight, eating a balanced diet low in fat, and avoiding excessive alcohol consumption. Regular exercise also supports overall health and can help prevent inflammation.
If doxycycline is unavoidable, discuss alternative antibiotics with your doctor. Tetracyclines like minocycline may be considered, but each antibiotic has its own potential side effects, including pancreatitis risk. Your physician will weigh the benefits and risks based on your specific health condition and needs.
Always inform your doctor about your medical history, including any previous instances of pancreatitis or liver problems, before starting any antibiotic. This allows for a more tailored approach to treatment and helps avoid potential complications.
Careful monitoring of liver and pancreatic enzymes is crucial during antibiotic treatment. Report any abdominal pain, nausea, vomiting, or jaundice immediately to your healthcare provider. Early intervention significantly improves outcomes.
Consider your individual risk factors. Patients with pre-existing conditions like gallstones or autoimmune diseases may be at higher risk of pancreatitis from doxycycline and require particularly close monitoring or alternative treatments.
Remember, this information is for general knowledge and does not constitute medical advice. Always consult with your healthcare provider for diagnosis and treatment of any medical condition.