If your urinary tract infection (UTI) isn’t clearing up with Ciprofloxacin, don’t panic. This isn’t uncommon. Antibiotic resistance is a growing concern, and Cipro is a frequently prescribed antibiotic, leading to increased resistance in certain bacteria strains. Let’s explore potential next steps.
First, schedule a follow-up appointment with your doctor immediately. They need to reassess your symptoms and potentially order further tests. This might include a urine culture to identify the specific bacteria causing the infection and determine its antibiotic susceptibility.
Second, accurately report all your symptoms. Detail the duration, intensity, and type of pain or discomfort. Mention any other symptoms like fever, chills, or changes in urination frequency or color. This helps your doctor tailor the right treatment plan for you.
Third, consider lifestyle factors. Adequate hydration is key for flushing out bacteria. Avoid irritants like caffeine and alcohol, which can exacerbate symptoms. Your doctor might also recommend specific dietary changes based on your individual situation.
Remember: Never adjust or stop your medication without consulting your doctor. Self-treating a UTI can lead to severe complications. Following your doctor’s guidance is crucial for effective treatment and preventing future infections.
Note: This information is for educational purposes only and doesn’t replace professional medical advice. Always consult your doctor before making any decisions about your health.
- Uti Not Responding to Cipro: What to Do
- Understanding Resistance
- Alternative Treatments
- Managing Symptoms
- Prevention
- Serious Considerations
- Understanding Ciprofloxacin Resistance in UTIs
- Factors Driving Resistance
- Combating Resistance
- Alternative Treatment Options
- Alternative Antibiotics for Cipro-Resistant UTIs
- Augmentin and Other Options
- Diagnosing the Cause of Treatment Failure
- Identifying Potential Contributing Factors
- Alternative Treatment Strategies
- Lifestyle Changes to Support UTI Treatment
- When to Seek Urgent Medical Attention
- Signs Requiring Immediate Attention:
- When to Contact Your Doctor:
- Remember:
Uti Not Responding to Cipro: What to Do
First, schedule a follow-up appointment with your doctor immediately. Don’t delay.
Your doctor needs to re-evaluate your situation. They might order further tests, such as a urine culture to identify the specific bacteria causing the infection and determine its antibiotic sensitivity. This helps pinpoint the right treatment.
Understanding Resistance
Antibiotic resistance is a serious problem. Some bacteria naturally resist certain antibiotics, and others develop resistance over time. This means Ciprofloxacin might not be effective against your specific infection.
Alternative Treatments
Based on the test results, your doctor will prescribe a different antibiotic. This could be another fluoroquinolone, or a completely different class of antibiotics, such as a cephalosporin, nitrofurantoin, or trimethoprim-sulfamethoxazole. Your doctor will choose the most appropriate option for your specific case and medical history.
Managing Symptoms
While awaiting results and a new treatment, focus on symptom management. Drink plenty of fluids to flush out bacteria. Over-the-counter pain relievers, like ibuprofen or acetaminophen, can help alleviate discomfort. However, always check with your doctor before taking any medication, especially if you have pre-existing conditions.
Prevention
To prevent future UTIs, practice good hygiene. Wipe front to back after using the restroom. Drink plenty of water throughout the day. Urinate frequently, and don’t hold your urine. Consider cranberry supplements, but discuss their use with your doctor. Proper hydration and hygiene are key!
Serious Considerations
If you experience severe symptoms like high fever, chills, back pain, or nausea, seek immediate medical attention. These could indicate a more serious kidney infection.
Understanding Ciprofloxacin Resistance in UTIs
Ciprofloxacin resistance in urinary tract infections (UTIs) is a growing concern. Several factors contribute to this resistance. Bacteria, like E. coli, a frequent UTI culprit, can develop mutations that allow them to survive ciprofloxacin’s effects. These mutations often involve changes in genes coding for enzymes that break down the antibiotic or alter the antibiotic’s target site within the bacteria.
Factors Driving Resistance
Overuse of ciprofloxacin, both in human and veterinary medicine, significantly accelerates resistance development. Broad-spectrum antibiotic use disrupts the natural bacterial balance, favoring resistant strains. Poor infection control practices in healthcare settings further contribute to the spread of resistant bacteria. Patient non-compliance with prescribed antibiotic regimens also plays a role; incomplete courses allow resistant bacteria to survive and multiply.
Combating Resistance
Appropriate antibiotic stewardship is vital. Doctors should only prescribe ciprofloxacin when necessary, after confirming the bacterial species and its susceptibility to the drug via culture and sensitivity testing. Public health initiatives promoting hygiene and infection control are also crucial. Development and implementation of novel antimicrobial strategies, including alternative antibiotics and non-antibiotic therapies, are needed to fight resistant UTIs. Prompt diagnosis and treatment with the most effective antibiotic, guided by laboratory testing, are essential for improved patient outcomes.
Alternative Treatment Options
If ciprofloxacin proves ineffective, alternative antibiotics, such as nitrofurantoin or fosfomycin, may be considered. The choice of antibiotic depends on the specific bacteria causing the infection and the patient’s health status. In severe cases, hospitalization and intravenous antibiotics might be necessary. Remember, always consult a healthcare professional for diagnosis and treatment of UTIs.
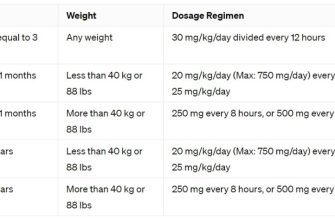
Alternative Antibiotics for Cipro-Resistant UTIs
If ciprofloxacin isn’t working for your UTI, your doctor might prescribe alternative antibiotics. Common options include nitrofurantoin, trimethoprim-sulfamethoxazole (TMP-SMX), or fosfomycin. Nitrofurantoin is generally well-tolerated and effective for uncomplicated UTIs. However, it’s not suitable for kidney problems. TMP-SMX offers a broad spectrum of activity but resistance is increasing, so susceptibility testing is vital. Fosfomycin is a single-dose treatment often used for uncomplicated UTIs. It’s a good choice when rapid treatment is needed.
Augmentin and Other Options
For more severe or complicated UTIs, your doctor may consider Augmentin (amoxicillin-clavulanate), a combination antibiotic effective against many bacterial strains. Other options include cephalosporins (like cefixime or cefpodoxime) or carbapenems (like imipenem or meropenem), typically reserved for resistant infections. Always discuss potential side effects and drug interactions with your physician before starting any medication.
Diagnosing the Cause of Treatment Failure
First, confirm the correct diagnosis. A misdiagnosis of the initial infection is a primary reason for ciprofloxacin failure. Retest the urine and/or other samples using different culture methods to rule out any errors.
Identifying Potential Contributing Factors
Next, investigate potential reasons for treatment resistance. This involves a multi-pronged approach:
- Bacterial Resistance Testing: Conduct antibiotic susceptibility testing (AST) to determine the Minimum Inhibitory Concentration (MIC) of ciprofloxacin against the isolated bacteria. This identifies the level of resistance.
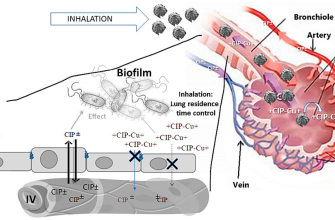
- Biofilm Formation: E. coli and other UTI-causing bacteria can form biofilms, shielding them from antibiotics. Consider this if standard treatment fails. Specific tests can assess biofilm production.
- Patient Factors: Evaluate patient adherence to the prescribed dosage and duration. Incomplete treatment allows bacteria to survive and potentially develop resistance.
- Co-infections: A secondary infection could be contributing to the treatment failure. Explore the possibility through additional testing.
- Drug Interactions: Review the patient’s medication history for potential interactions that could affect ciprofloxacin’s efficacy. Some medications interfere with absorption or metabolism.
- Host Immune Response: A weakened immune system could impair the body’s ability to clear the infection, even with effective antibiotic therapy. Assess the patient’s immune status.
Alternative Treatment Strategies
Based on the findings, a tailored treatment plan is essential. Options include:
- Different Antibiotic: If resistance is confirmed, select an alternative antibiotic based on the AST results. This might involve using a drug from a different class.
- Combination Therapy: Using two antibiotics simultaneously can be effective in overcoming resistance. Your doctor will choose appropriate combinations.
- Extended Treatment Duration: A longer course of antibiotics may be required in cases of slow eradication or suspected biofilm involvement.
Remember, accurate diagnosis and detailed investigation are crucial for successful treatment. Consult with a healthcare professional to discuss the best course of action.
Lifestyle Changes to Support UTI Treatment
Drink plenty of water – aim for at least eight glasses a day. This helps flush out bacteria from your urinary tract.
Cranberry juice can be beneficial. Studies suggest it may prevent bacteria from adhering to the bladder walls. Opt for unsweetened varieties.
Avoid irritants. Limit caffeine, alcohol, and sugary drinks, which can aggravate bladder inflammation.
Practice good hygiene. Always wipe from front to back after using the restroom to prevent bacteria from entering the urethra.
Wear breathable clothing. Tight-fitting clothing can trap moisture and increase the risk of infection.
Empty your bladder completely when you urinate. Don’t hold your urine for extended periods.
Consider probiotics. Some research indicates certain probiotics may support urinary tract health. Discuss this with your doctor before taking them.
| Change | Benefit |
|---|---|
| Increased water intake | Flushing out bacteria |
| Cranberry juice (unsweetened) | Preventing bacterial adhesion |
| Reducing irritants | Decreasing bladder inflammation |
| Proper hygiene | Preventing bacterial entry |
| Breathable clothing | Reducing moisture retention |
| Complete bladder emptying | Minimizing bacterial growth |
| Probiotics (consult doctor) | Supporting urinary tract health |
These lifestyle changes, combined with prescribed medication, can significantly aid your recovery. Always consult your doctor for personalized advice and to rule out any complications.
When to Seek Urgent Medical Attention
If your UTI symptoms worsen significantly despite taking Cipro, seek immediate medical care. This includes experiencing severe pain, high fever (over 101°F or 38.3°C), chills, or blood in your urine.
Signs Requiring Immediate Attention:
- Severe abdominal or flank pain
- Inability to urinate
- Fever above 101°F (38.3°C)
- Chills and shaking
- Blood in your urine
- Nausea and vomiting
These symptoms could indicate a serious kidney infection or other complications. Don’t delay; contact your doctor or go to the emergency room.
When to Contact Your Doctor:
- No improvement in symptoms after 72 hours of Ciprofloxacin treatment.
- Symptoms are not fully resolving after the prescribed course of antibiotics.
- You experience new or worsening symptoms alongside your UTI.
- You have concerns about your treatment or the side effects of Ciprofloxacin.
Your doctor can assess your situation, determine the cause of the ongoing infection, and adjust your treatment plan accordingly. Open communication with your healthcare provider is key to managing your UTI effectively.
Remember:
This information is for guidance only and should not replace professional medical advice. Always consult your doctor for diagnosis and treatment.