No, amoxicillin won’t treat hemorrhoids. Amoxicillin is an antibiotic, targeting bacterial infections. Hemorrhoids, however, are swollen veins in the anus and rectum, caused by increased pressure. This means a different approach is needed.
Instead of antibiotics, focus on lifestyle changes and over-the-counter treatments. Consider increasing fiber intake to soften stools, reducing straining during bowel movements. Warm baths can soothe inflamed hemorrhoids, providing immediate relief. Topical creams containing hydrocortisone or lidocaine can also alleviate discomfort and reduce swelling. For persistent or severe symptoms, consult a doctor; they can recommend stronger treatments or suggest further investigation.
Remember, self-treating can be risky. Proper diagnosis is crucial for effective management. A healthcare professional can accurately assess your condition and recommend the most appropriate treatment plan, tailored to your specific needs. Ignoring symptoms or using incorrect medications might delay healing and potentially worsen the condition.
Key takeaway: Amoxicillin is ineffective against hemorrhoids. Prioritize lifestyle adjustments, over-the-counter remedies, and, if necessary, seek professional medical advice for effective hemorrhoid management.
- Amoxicillin for Hemorrhoids: A Detailed Overview
- Understanding Hemorrhoids and Their Causes
- Pressure Increases: Key Factors
- Other Contributing Factors
- Amoxicillin: Its Mechanism and Uses
- Spectrum of Activity
- Important Considerations
- Does Amoxicillin Treat Hemorrhoid Symptoms?
- Potential Risks and Side Effects of Amoxicillin
- Alternative Treatments for Hemorrhoids
- Topical Treatments
- Other Approaches
- When to See a Doctor
- Disclaimer:
- When to See a Doctor for Hemorrhoid Treatment
- Home Remedies for Hemorrhoid Relief
- Preventing Hemorrhoids: Lifestyle and Dietary Changes
- Dietary Adjustments for Hemorrhoid Prevention
- Lifestyle Modifications
- Specific Dietary Recommendations
Amoxicillin for Hemorrhoids: A Detailed Overview
Amoxicillin is an antibiotic, targeting bacterial infections. It does not treat hemorrhoids, which are swollen veins in the anus and rectum. Hemorrhoids stem from increased pressure in these veins, often due to straining during bowel movements, pregnancy, or prolonged sitting.
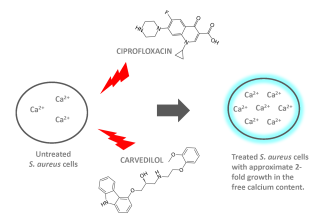
If you experience a hemorrhoid infection (e.g., a thrombosed hemorrhoid with a secondary bacterial infection), your doctor might prescribe antibiotics *in addition to* hemorrhoid treatment. Amoxicillin might be one option, but other antibiotics may be more appropriate depending on the specific bacteria causing the infection. The choice depends on factors like the type of infection and any allergies you have.
Treating the underlying hemorrhoid is crucial. This typically involves strategies to soften stool, such as increased fiber intake and hydration. Over-the-counter creams and suppositories can offer temporary relief from pain and itching. For severe cases, your doctor might recommend more advanced treatments, including procedures to reduce hemorrhoid size or band ligation.
Never self-treat a suspected hemorrhoid infection. A proper diagnosis and personalized treatment plan from a healthcare professional are necessary to ensure appropriate antibiotic use and address the underlying hemorrhoid condition.
Ignoring a possible infection can lead to complications. Seek medical attention if you experience symptoms like severe pain, bleeding, or a noticeable increase in swelling.
Understanding Hemorrhoids and Their Causes
Hemorrhoids, or piles, are swollen veins in the anus and rectum. They develop when increased pressure affects the blood vessels in this area.
Pressure Increases: Key Factors
Several factors contribute to this increased pressure. Straining during bowel movements is a primary cause. Chronic constipation significantly raises this risk, as does prolonged sitting or standing. Pregnancy frequently leads to hemorrhoids due to the pressure of the growing uterus on pelvic veins. Obesity also increases pressure within the abdomen.
Other Contributing Factors
Beyond pressure, low-fiber diets lead to harder stools, requiring more straining. Lifting heavy objects regularly puts significant strain on the pelvic area. Aging weakens connective tissues, making veins more prone to swelling. Certain medical conditions, like liver disease, can also increase the likelihood of developing hemorrhoids.
Amoxicillin: Its Mechanism and Uses
Amoxicillin is a penicillin-derived antibiotic. It works by inhibiting bacterial cell wall synthesis, preventing bacterial growth and ultimately leading to bacterial death. This mechanism targets bacteria, not the human body.
Spectrum of Activity
Amoxicillin effectively treats a wide range of bacterial infections. Common targets include infections of the respiratory tract (pneumonia, bronchitis), ears (otitis media), skin, urinary tract, and certain sexually transmitted infections. However, its effectiveness varies depending on the specific bacteria causing the infection. Some bacteria have developed resistance.
Important Considerations
Amoxicillin is a prescription drug. Always follow your doctor’s instructions regarding dosage and duration of treatment. Allergic reactions, while rare, can be serious. Common side effects include diarrhea, nausea, and skin rash. Inform your doctor about any allergies or medical conditions before taking amoxicillin. Amoxicillin does not treat viral infections like the common cold or influenza. Antibiotic misuse contributes to antibiotic resistance, a significant public health concern.
Does Amoxicillin Treat Hemorrhoid Symptoms?
No, amoxicillin does not treat hemorrhoid symptoms. Amoxicillin is an antibiotic, targeting bacterial infections. Hemorrhoids, on the other hand, are swollen veins in the anus and rectum, not caused by bacteria.
Treating the pain and inflammation associated with hemorrhoids requires different approaches. Over-the-counter treatments like creams, suppositories, or ointments containing hydrocortisone or lidocaine can provide relief from pain and itching. Sitz baths (soaking in warm water) can also ease discomfort.
For more severe hemorrhoids, a doctor might recommend stronger medications or procedures such as rubber band ligation or surgical removal. If you experience severe bleeding, persistent pain, or other concerning symptoms, seek medical attention immediately. A healthcare professional can properly diagnose your condition and recommend the appropriate treatment plan.
Potential Risks and Side Effects of Amoxicillin
Amoxicillin, while generally safe, can cause side effects. Common reactions include diarrhea, nausea, and vomiting. These usually are mild and resolve without intervention.
More serious, though less frequent, side effects include allergic reactions. These can range from mild skin rashes to severe, life-threatening anaphylaxis. Seek immediate medical attention if you experience swelling of the face, lips, or tongue, difficulty breathing, or hives after taking amoxicillin.
Amoxicillin can also disrupt gut flora, potentially leading to yeast infections, particularly in women. This manifests as vaginal itching or discharge. Contact your doctor if you suspect a yeast infection.
While rare, amoxicillin can affect liver function. Symptoms include jaundice (yellowing of the skin and eyes), dark urine, and abdominal pain. Report these symptoms to your doctor immediately.
Amoxicillin may interact with certain medications. Always inform your doctor or pharmacist about all medications, supplements, and herbal remedies you are taking. This helps avoid potential drug interactions.
This information is for general knowledge and does not substitute professional medical advice. Always consult your doctor before starting any medication, including amoxicillin, especially if you have pre-existing health conditions or are pregnant or breastfeeding.
Alternative Treatments for Hemorrhoids
Consider lifestyle changes first. Increase your fiber intake significantly – aim for 25-30 grams daily through fruits, vegetables, and whole grains. This softens stools, easing bowel movements and reducing strain.
Stay hydrated! Drink plenty of water throughout the day to help keep your stools soft and prevent constipation. Aim for at least eight glasses.
Topical Treatments
- Over-the-counter creams and ointments: Many products containing hydrocortisone or other soothing agents offer temporary relief from itching and pain. Follow package instructions carefully.
- Witch hazel: Soothes irritated skin and can reduce swelling. Apply directly to the affected area with a cotton ball.
- Aloe vera: Its anti-inflammatory properties can help reduce pain and inflammation. Use pure aloe vera gel.
Other Approaches
- Sitz baths: Soaking in warm water for 15-20 minutes several times a day can ease pain and inflammation. Add Epsom salts for extra relief.
- Cold compresses: Applying a cold compress to the affected area can help reduce swelling and numb the pain.
- Regular exercise: Maintaining a healthy weight reduces pressure on the veins in your rectum and anus.
When to See a Doctor
Persistent pain, bleeding, or other concerning symptoms warrant a medical evaluation. Your doctor can diagnose the issue and recommend appropriate treatment.
Disclaimer:
This information is for educational purposes only and does not constitute medical advice. Always consult your physician before starting any new treatment.
When to See a Doctor for Hemorrhoid Treatment
Schedule an appointment if your hemorrhoids don’t improve within a week of home treatment, or if symptoms worsen.
Seek immediate medical attention if you experience:
| Symptom | Description |
|---|---|
| Bright red bleeding | Heavy bleeding warrants immediate assessment. |
| Severe pain | Intense, unbearable pain requires professional evaluation. |
| Strangulated hemorrhoid | A hemorrhoid that’s cut off from blood supply, appearing dark purple or black, is a medical emergency. |
| Fever and chills | These may indicate an infection requiring antibiotics. |
| Anemia symptoms | Fatigue, dizziness, pale skin can suggest significant blood loss. |
Your doctor can diagnose the cause of your symptoms and recommend appropriate treatment options, including prescription medications stronger than over-the-counter remedies, minimally invasive procedures, or surgery.
Don’t hesitate to contact a healthcare professional if you have any concerns about your hemorrhoids. Early intervention often leads to better outcomes.
Home Remedies for Hemorrhoid Relief
Soothe inflammation with witch hazel. Apply a cool compress soaked in witch hazel directly to the affected area for 15-20 minutes several times daily. This helps reduce swelling and itching.
Epsom salt baths provide relief. Dissolve 1-2 cups of Epsom salts in a warm bath and soak for 15-20 minutes. The magnesium sulfate in Epsom salts can ease discomfort.
Ice packs reduce pain and swelling. Apply a cold pack wrapped in a thin cloth to the hemorrhoid for 10-15 minutes at a time. Repeat as needed for temporary pain relief.
Aloe vera gel offers a natural soothing agent. Apply a small amount of pure aloe vera gel directly to the hemorrhoid. Its anti-inflammatory properties can help calm irritated skin.
Maintain a high-fiber diet. Increase your intake of fruits, vegetables, and whole grains to promote regular bowel movements and prevent constipation, a major hemorrhoid trigger. Aim for at least 25-30 grams of fiber daily.
Drink plenty of water. Staying hydrated softens stools, making bowel movements easier and less straining. This reduces pressure on hemorrhoids.
Important Note: While these home remedies can offer temporary relief, consult a doctor if symptoms persist or worsen. They can provide a proper diagnosis and recommend appropriate treatment.
Preventing Hemorrhoids: Lifestyle and Dietary Changes
Maintain a healthy weight. Excess weight puts extra pressure on your veins, increasing your risk. Aim for a gradual weight loss through diet and exercise if needed.
Dietary Adjustments for Hemorrhoid Prevention
- Increase fiber intake: Aim for 25-30 grams of fiber daily. Include plenty of fruits, vegetables, and whole grains in your diet. This softens stools, making bowel movements easier and less straining.
- Drink plenty of fluids: Water keeps stools soft and prevents constipation. Aim for at least 8 glasses of water a day.
- Limit processed foods: These often lack fiber and can contribute to constipation.
- Reduce caffeine and alcohol: These can dehydrate you, hardening stools.
Lifestyle Modifications
- Regular exercise: Physical activity improves circulation and bowel regularity. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Avoid prolonged sitting or standing: Regularly change positions to improve blood flow. Take short breaks to walk around.
- Don’t strain during bowel movements: If you experience constipation, address it through diet and lifestyle changes, not straining.
- Practice good hygiene: Gently cleanse the anal area after bowel movements with soft toilet paper or wipes. Avoid harsh soaps or scrubbing.
Specific Dietary Recommendations
Consider incorporating these fiber-rich foods into your daily diet:
- Oats
- Beans
- Lentils
- Broccoli
- Berries
Remember to consult your doctor before making significant dietary or lifestyle changes, especially if you have pre-existing health conditions.