Ciprofloxacin (Cipro) is generally ineffective against Enterococcus faecalis infections. Resistance rates are high, meaning Cipro is unlikely to successfully treat the infection.
Instead of Cipro, clinicians typically prescribe antibiotics like ampicillin, vancomycin, or linezolid, depending on the specifics of the infection and the patient’s medical history. These antibiotics demonstrate significantly higher success rates in combating E. faecalis.
Always consult a healthcare professional for diagnosis and treatment. Self-treating an E. faecalis infection with Cipro or any other antibiotic without medical supervision can lead to serious complications, including the development of antibiotic-resistant strains and delayed treatment, potentially worsening the infection’s severity. Laboratory testing will determine the appropriate antibiotic.
E. faecalis infections are often hospital-acquired, affecting individuals with weakened immune systems. Prompt medical attention is crucial for optimal outcomes.
- Ciprofloxacin and Enterococcus faecalis: A Detailed Overview
- Resistance Mechanisms
- Treatment Implications
- Monitoring Treatment
- Understanding Enterococcus faecalis Infections
- Common Infection Sites and Symptoms
- Diagnosis and Treatment
- Preventing Infections
- Ciprofloxacin’s Mechanism of Action
- Ciprofloxacin Resistance in E. faecalis: Mechanisms and Prevalence
- Factors Influencing Treatment Outcomes with Ciprofloxacin
- Antibiotic Susceptibility Testing
- Patient-Specific Factors
- Treatment Regimen
- Monitoring and Adjustment
- Emerging Resistance
- Alternative Treatment Options for E. faecalis Infections
- Prevention Strategies for E. faecalis Infections
- Preventing Healthcare-Associated Infections
- Environmental Control Measures
- The Role of Diagnostics in Guiding Treatment Decisions
- Identifying the Infecting Strain
- Assessing the Infection Site and Severity
- Treatment Strategy Based on Diagnostic Results
- Monitoring Treatment Response
- Future Directions in Combating Ciprofloxacin-Resistant E. faecalis
- Developing Novel Antibiotics
- Combating Biofilm Formation
- Combination Therapies
- Monitoring and Surveillance
- Infection Control Measures
- Investigating Resistance Mechanisms
- Data-Driven Approaches
- Table 1: Key Research Areas
Ciprofloxacin and Enterococcus faecalis: A Detailed Overview
Ciprofloxacin’s effectiveness against Enterococcus faecalis is limited. Resistance is a significant concern. Many strains demonstrate inherent resistance, meaning they are naturally not susceptible to the antibiotic.
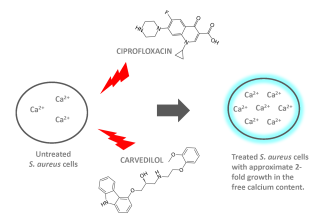
Resistance Mechanisms
E. faecalis employs several mechanisms to resist ciprofloxacin. These include mutations in topoisomerase IV and DNA gyrase, the enzymes targeted by the drug. Efflux pumps actively remove ciprofloxacin from the bacterial cell, reducing intracellular drug concentration. Decreased outer membrane permeability also hinders drug penetration.
Treatment Implications
Given the high prevalence of ciprofloxacin resistance, it’s rarely a first-line choice for E. faecalis infections. Susceptibility testing is crucial before prescribing. Alternative antibiotics such as ampicillin, vancomycin, or linezolid are frequently preferred. Treatment decisions should consider the specific infection site, patient factors, and the results of susceptibility testing. For serious infections, combination therapy may be necessary to overcome resistance.
Monitoring Treatment
Close monitoring of clinical response is vital during ciprofloxacin treatment (if used), as well as with alternative antibiotics. Regular follow-up appointments allow for timely adjustments in the treatment plan based on the patient’s response and any detected complications. Failure to respond to treatment may indicate resistance and necessitate a switch to a different antibiotic regimen.
Understanding Enterococcus faecalis Infections
Enterococcus faecalis is a resilient bacterium, frequently causing healthcare-associated infections. These infections are often resistant to multiple antibiotics, necessitating careful diagnosis and treatment planning. This resistance stems from inherent characteristics and the acquisition of resistance genes.
Common Infection Sites and Symptoms
E. faecalis most commonly infects the urinary tract, causing urinary tract infections (UTIs) characterized by pain during urination, frequent urination, and potentially fever. It can also cause bloodstream infections (bacteremia), often presenting with fever, chills, and low blood pressure. Endocarditis, an infection of the heart valves, is a severe complication, manifesting as fever, heart murmur, and shortness of breath. Wound infections following surgery or trauma are another significant concern; signs include localized pain, swelling, redness, and pus.
Diagnosis and Treatment
Diagnosing E. faecalis infections involves culturing samples from the infected site (urine, blood, wound). Antibiotic susceptibility testing is crucial to guide treatment. Ampicillin and vancomycin are common choices, but resistance necessitates the use of alternative antibiotics like linezolid or daptomycin. Treatment duration varies depending on the infection type and severity; close monitoring by healthcare professionals is paramount.
Preventing Infections
Preventing E. faecalis infections hinges on robust infection control practices in healthcare settings, including hand hygiene, sterile techniques during procedures, and appropriate antibiotic stewardship. Maintaining a healthy immune system also reduces susceptibility. Prompt treatment of existing infections prevents spread and reduces the risk of developing more severe complications.
Ciprofloxacin’s Mechanism of Action
Ciprofloxacin targets bacterial DNA gyrase and topoisomerase IV. These enzymes are crucial for DNA replication, transcription, and repair in bacteria.
- DNA Gyrase: Ciprofloxacin inhibits DNA gyrase, preventing the enzyme from supercoiling bacterial DNA. This supercoiling is necessary for DNA compaction and proper function. Inhibition leads to DNA breakage and cell death.
- Topoisomerase IV: Similarly, ciprofloxacin blocks topoisomerase IV, an enzyme essential for separating replicated DNA during bacterial cell division. This inhibition prevents the separation of daughter chromosomes, halting replication and causing cell death.
The precise mechanism involves ciprofloxacin binding to the enzyme-DNA complex, stabilizing a cleaved DNA intermediate. This blockage prevents religation and resealing of the DNA strand, leading to irreversible DNA damage.
Importantly, the impact of ciprofloxacin varies depending on the bacterial species. Enterococcus faecalis, for instance, exhibits varying levels of resistance, often due to mutations in the target enzymes or efflux pump mechanisms that actively remove the drug from the cell.
- Mutations in gyrA and parC genes, encoding DNA gyrase and topoisomerase IV subunits respectively, often confer resistance.
- Efflux pumps actively transport ciprofloxacin out of the bacterial cell, reducing intracellular drug concentration.
Understanding these mechanisms helps explain both ciprofloxacin’s efficacy and the development of resistance in bacteria like Enterococcus faecalis. Appropriate antibiotic stewardship practices are therefore crucial.
Ciprofloxacin Resistance in E. faecalis: Mechanisms and Prevalence
Enterococcus faecalis resistance to ciprofloxacin is a significant clinical challenge. Multiple mechanisms contribute to this resistance.
Mutations in the quinolone resistance-determining regions (QRDRs) of the gyrA and gyrB genes are common. These mutations alter the target enzyme, topoisomerase IV and DNA gyrase, reducing ciprofloxacin binding and efficacy. Studies show gyrA mutations occur more frequently than gyrB mutations. Specific mutations, like Ser83 to Leu in GyrA, are frequently associated with high-level resistance.
Efflux pumps actively remove ciprofloxacin from the bacterial cell. Increased expression of efflux pumps like NorA and MepA, often driven by mutations in regulatory genes, enhances this efflux, contributing to resistance. The prevalence of these efflux pump-mediated mechanisms varies geographically and according to the clinical setting.
Reduced outer membrane permeability also contributes to resistance. Altered membrane composition hinders ciprofloxacin entry into the cell. This mechanism often works synergistically with efflux pumps and QRDR mutations.
Prevalence data shows considerable variation globally. Resistance rates in nosocomial infections are substantially higher than those in community-acquired infections. Data from several studies consistently reports ciprofloxacin resistance rates in E. faecalis ranging from 10% to over 50%, depending on factors like geographical location, healthcare setting, and the time period of the study. These variations highlight the importance of local susceptibility data for appropriate antibiotic selection.
Understanding these diverse resistance mechanisms is crucial for developing strategies to combat ciprofloxacin-resistant E. faecalis infections. This includes targeted antibiotic stewardship programs promoting responsible antibiotic use and exploring alternative treatment options.
Factors Influencing Treatment Outcomes with Ciprofloxacin
Successful treatment of Enterococcus faecalis infections with ciprofloxacin hinges on several key factors. Minimizing resistance development is paramount.
Antibiotic Susceptibility Testing
Accurate susceptibility testing is crucial. Minimum inhibitory concentration (MIC) values directly influence treatment success. Higher MIC values predict treatment failure. Consider using tests like broth microdilution or Etest for precise MIC determination.
Patient-Specific Factors
- Immune Status: A weakened immune system hampers the body’s ability to fight the infection, negatively impacting treatment outcomes. Immunocompromised patients may require longer treatment durations or combination therapy.
- Infection Site: Deep-seated infections, like endocarditis, are harder to treat than superficial infections. Antibiotic penetration to the infection site is critical. Consider alternative treatment options if penetration is insufficient.
- Age and Renal Function: Older patients and individuals with renal impairment require dose adjustments to prevent toxicity. Reduced renal clearance increases drug accumulation, potentially leading to side effects. Close monitoring of creatinine levels is recommended.
- Drug Interactions: Concurrent use of medications that interact with ciprofloxacin can affect its efficacy. Consult drug interaction databases to identify potential problems.
Treatment Regimen
- Dosage and Duration: Appropriate dosage and treatment duration are crucial. Consult current treatment guidelines to determine optimal parameters based on the infection severity and patient characteristics.
- Combination Therapy: For severe infections or those caused by resistant strains, consider combining ciprofloxacin with other antibiotics, like ampicillin or vancomycin. This synergistic approach can enhance efficacy.
- Adherence: Patient adherence to the prescribed treatment regimen is essential. Non-compliance reduces the chance of successful eradication of the infection.
Monitoring and Adjustment
Regular clinical monitoring is vital. Assess the patient’s response to treatment, including symptom resolution and laboratory test results. Adjust the treatment strategy as needed based on clinical response and microbiological data. Failure to improve warrants reevaluation and potential regimen change.
Emerging Resistance
Ciprofloxacin resistance in Enterococcus faecalis is an increasing concern. Strategies to limit resistance spread include judicious antibiotic use, infection control measures, and exploring alternative treatment options when resistance is confirmed.
Alternative Treatment Options for E. faecalis Infections
Consider linezolid as a viable alternative. This antibiotic often proves effective against resistant strains.
Daptomycin offers another strong option, particularly for serious infections. Its mechanism of action differs from many other antibiotics, making it a valuable choice when other treatments fail.
Tigecycline represents a broad-spectrum antibiotic, useful in cases of multi-drug resistance. However, remember to carefully weigh potential side effects.
For localized infections, surgical debridement may be necessary. Removal of infected tissue allows for better antibiotic penetration.
Bacteriophage therapy, using viruses that specifically target E. faecalis, shows promise but remains largely investigational. Clinical trials are ongoing, and this may become a more established treatment in the future.
Always consult an infectious disease specialist for personalized treatment recommendations. They can accurately assess your specific situation and select the best approach, considering factors like the severity of the infection, antibiotic susceptibility testing results, and your overall health.
Prevention Strategies for E. faecalis Infections
Maintain meticulous hygiene practices. Wash your hands frequently with soap and water, especially after using the restroom and before handling food. Hand sanitizers containing at least 60% alcohol are also effective between washings.
Properly sterilize medical equipment. Adherence to strict sterilization protocols in healthcare settings significantly reduces the risk of E. faecalis transmission. This includes thorough cleaning and disinfection of instruments and surfaces.
Practice safe sex. Using barrier methods like condoms lowers the risk of sexually transmitted infections, including those caused by E. faecalis.
Preventing Healthcare-Associated Infections
Antibiotic stewardship is paramount. Careful antibiotic prescription by healthcare providers helps prevent the development of antibiotic-resistant strains of E. faecalis. Avoid unnecessary antibiotic use.
Isolate infected patients. Implementing appropriate infection control measures, such as contact precautions, in hospitals and healthcare facilities isolates infected individuals, minimizing the spread of E. faecalis to other patients.
Environmental Control Measures
Regular disinfection of surfaces is key. Frequently disinfect frequently touched surfaces, especially in healthcare and high-traffic areas. This includes doorknobs, countertops, and shared equipment.
Careful waste disposal is crucial. Medical waste containing potentially infectious materials should be disposed of according to established guidelines to prevent contamination and spread.
| Strategy | Description |
|---|---|
| Hand Hygiene | Frequent handwashing with soap and water, or alcohol-based sanitizer. |
| Sterilization | Thorough sterilization of medical equipment and surfaces. |
| Safe Sex Practices | Condom use to prevent transmission of sexually transmitted infections. |
| Antibiotic Stewardship | Judicious use of antibiotics to prevent resistance. |
| Patient Isolation | Isolation of infected patients to limit spread. |
| Environmental Disinfection | Regular disinfection of frequently touched surfaces. |
| Waste Disposal | Proper disposal of medical waste. |
The Role of Diagnostics in Guiding Treatment Decisions
Accurate diagnosis is paramount for effective Enterococcus faecalis treatment. Ciprofloxacin resistance is common, so relying solely on susceptibility testing is insufficient. We need a multifaceted approach.
Identifying the Infecting Strain
- Gram staining and culture: Confirm the presence of E. faecalis. This initial step is crucial for guiding antibiotic selection.
- Susceptibility testing: Determine antibiotic sensitivities using methods like broth microdilution or disk diffusion. This identifies effective alternatives to Ciprofloxacin.
- PCR-based methods: Detect specific resistance genes, like those encoding for aminoglycoside-modifying enzymes or vancomycin resistance. This helps predict treatment outcome.
Assessing the Infection Site and Severity
The location and severity of infection significantly influence treatment choice.
Treatment Strategy Based on Diagnostic Results
- Susceptible E. faecalis: Use appropriate antibiotics based on susceptibility results. Consider factors like patient allergies and potential side effects.
- Resistant E. faecalis: This necessitates a shift to alternative treatment strategies. Options might include combination therapy with synergistic antibiotics or surgery in severe cases.
- High-risk patients (immunocompromised): Require more aggressive treatment approaches, possibly including prolonged antibiotic courses and close monitoring for complications.
Monitoring Treatment Response
- Clinical evaluation: Monitor patient symptoms and vital signs to assess the treatment’s effectiveness.
- Repeat cultures: Obtain repeat cultures to confirm eradication of the infection and assess for the emergence of resistance.
This diagnostic-guided approach improves treatment outcomes and minimizes the risk of treatment failure.
Future Directions in Combating Ciprofloxacin-Resistant E. faecalis
Prioritize research into alternative therapeutic strategies. This includes exploring novel antibiotic targets within E. faecalis, focusing on mechanisms distinct from those affected by ciprofloxacin. Investigate the potential of bacteriophage therapy, leveraging naturally occurring viruses to target and eliminate resistant strains.
Developing Novel Antibiotics
Direct efforts toward developing new antibiotics with unique mechanisms of action to circumvent existing resistance mechanisms. This should involve high-throughput screening of diverse chemical libraries and advanced computational methods for drug design. Target specific bacterial processes such as cell wall synthesis or DNA replication, areas less impacted by existing resistance.
Combating Biofilm Formation
E. faecalis biofilms significantly contribute to antibiotic resistance. Research should focus on developing anti-biofilm strategies, including compounds that disrupt biofilm formation or enhance antibiotic penetration into established biofilms. This could involve targeting specific signaling pathways or enzymes involved in biofilm development.
Combination Therapies
Explore synergistic combinations of existing and novel antibiotics with other antimicrobial agents, such as bacteriophages or existing drugs targeting different bacterial pathways. This approach can potentially overcome resistance and improve treatment efficacy. Preclinical and clinical trials should carefully evaluate the efficacy and safety of these combinations.
Monitoring and Surveillance
Strengthen global surveillance systems to track the spread of ciprofloxacin-resistant E. faecalis. This necessitates robust laboratory capacity for accurate and timely detection of resistant strains and improved data sharing between healthcare systems worldwide. Accurate epidemiological data is key to directing effective intervention strategies.
Infection Control Measures
Implement and rigorously enforce infection control measures in healthcare settings to limit the spread of resistant strains. This includes appropriate hand hygiene, meticulous sterilization protocols, and the prudent use of antibiotics. Focus should also be on identifying and treating carriers of resistant strains.
Investigating Resistance Mechanisms
Conduct comprehensive genomic analyses to identify novel resistance mechanisms in ciprofloxacin-resistant E. faecalis. This information can be invaluable for guiding the development of new therapeutic strategies and predictive diagnostics.
Data-Driven Approaches
Utilize advanced bioinformatics and machine learning techniques to analyze large datasets on antibiotic resistance. These tools can help to predict the emergence of resistance, identify potential therapeutic targets, and guide the development of personalized treatment strategies.
Table 1: Key Research Areas
| Area | Specific Focus |
|---|---|
| Antibiotic Discovery | Novel targets, high-throughput screening |
| Biofilm Disruption | Signal pathway inhibitors, enzymatic disruption |
| Combination Therapies | Bacteriophage-antibiotic combinations |
| Surveillance | Genomic sequencing, global data sharing |