Don’t mix clindamycin and amoxicillin without consulting your doctor. Simultaneous use can negatively impact the effectiveness of both antibiotics, potentially leading to treatment failure and antibiotic resistance.
Clindamycin and amoxicillin target different bacteria. Amoxicillin is a penicillin-type antibiotic, while clindamycin belongs to the lincosamide class. Using them together may not provide additional benefits and could cause unnecessary side effects. Your physician needs to evaluate your specific infection and determine the optimal antibiotic therapy.
Potential drug interactions exist; therefore, always disclose all medications you’re taking to your doctor or pharmacist. This includes over-the-counter drugs, supplements, and herbal remedies. Accurate information ensures your safety and treatment efficacy.
If you experience any unusual side effects such as severe diarrhea, allergic reactions (rash, itching, swelling), or difficulty breathing, seek immediate medical attention. Reporting adverse reactions helps healthcare professionals track potential issues associated with antibiotic use.
- Mixing Clindamycin and Amoxicillin: A Detailed Guide
- Why You Shouldn’t Combine Clindamycin and Amoxicillin Without Medical Supervision
- Specific Situations Where Combining Might Be Considered (Under Strict Medical Guidance)
- Severe Infections Requiring Broad-Spectrum Coverage
- Situations Where Monotherapy Fails
- Important Considerations:
- What to Do If You’ve Accidentally Taken Both Medications
Mixing Clindamycin and Amoxicillin: A Detailed Guide
Generally, combining clindamycin and amoxicillin isn’t recommended without a doctor’s explicit instruction. These antibiotics target different bacterial types, and simultaneous use might lead to unexpected drug interactions or reduced effectiveness of either medication.
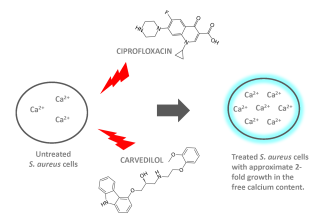
Amoxicillin, a penicillin-type antibiotic, effectively treats infections caused by susceptible bacteria. Clindamycin, a lincosamide, combats a broader range of bacteria, including some resistant to penicillin. However, taking both simultaneously can increase the risk of Clostridium difficile infection (C. diff), a serious complication characterized by severe diarrhea and colitis.
Specific interactions are possible. For example, concurrent use might alter the absorption or metabolism of either drug. Consequently, your doctor needs to carefully weigh the benefits against the potential risks in your individual case.
Always inform your doctor and pharmacist about all medications, including over-the-counter drugs and supplements, you’re taking before starting any new treatment. They can assess potential drug interactions and adjust the treatment plan accordingly. Accurate reporting ensures the safest and most effective therapy.
If experiencing any adverse effects such as diarrhea, nausea, vomiting, rash, or unusual fatigue after combining these antibiotics, contact your healthcare provider immediately. Prompt reporting ensures timely intervention and management of potential complications.
This information serves as guidance only and should not replace professional medical advice. Always consult your physician before altering your medication regimen.
Why You Shouldn’t Combine Clindamycin and Amoxicillin Without Medical Supervision
Avoid combining clindamycin and amoxicillin without your doctor’s explicit guidance. This is because these antibiotics, while both fighting bacterial infections, can interact in unexpected ways.
Increased Risk of Clostridium difficile Infection (CDI): Clindamycin disrupts the gut’s natural bacteria balance, increasing your susceptibility to C. difficile, a serious infection causing severe diarrhea. Amoxicillin, while generally less likely to cause CDI than clindamycin, can contribute to this risk if used concurrently.
Reduced Effectiveness: Combining these antibiotics might not enhance their effect as anticipated, and it could even lessen the effectiveness of either or both. Different antibiotics work through diverse mechanisms, and simultaneous use doesn’t guarantee a synergistic effect. Your doctor needs to assess if a combined approach is truly beneficial in your specific case.
Adverse Drug Reactions: Although uncommon, taking both medications simultaneously can lead to increased chances of side effects, such as nausea, vomiting, diarrhea, or skin rashes. Your body processes these drugs differently, and the combined effect might be unpredictable.
Always consult your physician before starting or changing antibiotic treatment. They can help determine the most appropriate antibiotic(s) and dosage for your infection, minimizing the risk of adverse reactions and maximizing treatment success. Ignoring this advice could lead to complications and prolong your recovery.
Specific Situations Where Combining Might Be Considered (Under Strict Medical Guidance)
Combining clindamycin and amoxicillin is rarely done and only under a doctor’s explicit instruction. This decision rests on a careful evaluation of the patient’s specific condition and potential benefits versus risks.
Severe Infections Requiring Broad-Spectrum Coverage
In cases of severe, polymicrobial infections – infections caused by multiple bacteria – a physician might prescribe this combination. For example:
- Certain severe skin and soft tissue infections (SSTIs) where both Gram-positive (susceptible to clindamycin) and Gram-negative (potentially susceptible to amoxicillin) bacteria are present.
- Specific types of intra-abdominal infections exhibiting a complex bacterial profile.
The choice depends on individual susceptibility testing results. Simply put, the doctor must confirm that the bacteria involved are likely responsive to this combination before prescribing.
Situations Where Monotherapy Fails
If a patient has a severe infection unresponsive to initial monotherapy with either amoxicillin or clindamycin, a doctor might consider adding the other antibiotic. This is a strategy of last resort. This change would be supported by:
- Culture and sensitivity testing showing resistance to the initial antibiotic.
- A clear clinical indication of ongoing infection despite initial treatment.
Important Considerations:
Remember: This combination increases the risk of side effects. The doctor will carefully weigh the potential benefits against the increased chance of complications such as Clostridium difficile-associated diarrhea (CDAD), liver problems, or allergic reactions. Regular monitoring is crucial in these cases.
What to Do If You’ve Accidentally Taken Both Medications
Contact your doctor or pharmacist immediately. Explain the situation clearly: the medications you took, the dosages, and the time you ingested them. They can assess the potential risks and advise on the best course of action.
Be prepared to provide details about your medical history, including any allergies or pre-existing conditions. This information is critical for them to make an informed decision.
Follow their instructions carefully. This might involve monitoring for any adverse reactions, such as nausea, vomiting, or diarrhea. You may be asked to visit the emergency room or undergo specific tests.
Do not attempt to self-treat or counteract the medication effects without professional guidance. This could potentially worsen the situation.
Keep a record of all communication with your healthcare provider, including the date, time, and specific instructions. This documentation will be helpful for future reference.
Drink plenty of fluids to help your body process the medications. However, avoid alcohol and other substances that could interact negatively with the drugs.